The case of the 30-year-old woman, who has not been publicly identified, is described in a new report published in the Annals of Internal Medicine. The woman was diagnosed with HIV in 2013, according to the study, and now shows no active signs of infection or intact HIV in large numbers of her cells. This, the researchers say, implies that she may have been able to achieve what's called a "sterilizing cure" of her HIV infection.
 Woman Cured of HIV (CDC). If the virus is not treated, it can lead to acquired immunodeficiency syndrome (AIDS). There is no effective cure for HIV, the CDC says, and people with the virus typically live with it in them for the rest of their lives. The 30-year-old woman seems to be an exception.
Woman Cured of HIV (CDC). If the virus is not treated, it can lead to acquired immunodeficiency syndrome (AIDS). There is no effective cure for HIV, the CDC says, and people with the virus typically live with it in them for the rest of their lives. The 30-year-old woman seems to be an exception.
To reach that conclusion, researchers analyzed blood samples collected from the woman between 2017 and 2020, along with placental tissue when she had a baby in March 2020. The woman didn't undergo any treatment until 2019 during her pregnancy, when she took the antiretroviral drugs tenofovir, emtricitabine, and raltegravir for six months. After she had her baby (who was HIV-negative), the woman stopped taking the medications.
RELATED: 16 HIV Symptoms Every Woman Needs to Know
And yes, notice the quotes around cure. "By 'cure,' we mean that there is no trace of virus in her body that is able to replicate and generate new viruses," lead study author Gabriela Turk, PhD, of the University of Buenos Aires, tells Health. "Instead, we only found seven copies—an extremely low number—of defective viruses; no signs of active infection or intact virus capable of replicating."
The woman is only the second patient who has achieved a "sterilizing cure" from HIV without undergoing a stem cell transplant (which has been shown to "cure" a few people in the past) or other treatment. The first person, 67-year-old Loreen Willenberg, has also been featured in research. Her body has suppressed HIV for decades after she was diagnosed with the virus in 1992, per The New York Times. In these very rare cases, doctors have referred to the patients as "elite controllers," infectious disease expert Amesh A. Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, tells Health.
How is it possible to be ‘cured’ of HIV in this way?
The short answer is that researchers just don't know. What is known is that "it is the patient's immune system that is doing it," Dr. Yu says. "We believe that multiple components of the immune system contribute, such as T cells and innate immune cells," she adds.
"The main hypothesis is that natural immunity played its part," study co-author Natalia Laufer, MD, PhD, of the University of Buenos Aires, tells Health. "The next challenge is to figure out how it was achieved and try to understand the immune mechanisms that were involved. If this task might have been accomplished, there might be a chance to generate a therapy to recapitulate to same effect in every [person] living with HIV."
RELATED: This 29-Year-Old Went to the Doctor for a Rash—and It Turned Out He Had HIV
How is a ‘sterilizing cure’ different from taking medicine and achieving a level of disease that is undetectable?
While contracting HIV used to mean that a person would eventually develop AIDS and die of the condition within a few years, HIV can now be controlled with medications that can slow or prevent the progression of the virus. With daily, lifelong antiretroviral therapy (ART), the amount of HIV in an infected person's blood might be made so small that the virus isn't detectable on a standard blood test.
The difference between what happened with this patient and what happens to the vast majority of people who take ART is that HIV treatment only suppresses the virus; it doesn't eliminate it, according to Dr. Yu. "In our patient, there is no intact virus detectable any more, despite analyzing massive amounts of cells," she says. So even though the patient took ART for six months, that alone wouldn't have cured her. In fact, for those taking ART, "HIV persists and comes back as soon as they stop the medicine," according to Dr. Yu.
When HIV gets into the body, it immediately starts making more of itself, John Nelson, PhD, HIV expert and researcher at the Rutgers School of Nursing, tells Health. "The medications are kind of like birth control pills for HIV," he explains. "They prevent, in different ways, the replication of the virus. But people on these medications aren't cured until that HIV that's incorporated into the DNA is completely eliminated. We recommend that all persons with HIV go on medication as soon as they can and stay on the medication for the rest of their life until we find the cure."
Not taking medication will allow higher levels of HIV to circulate in the blood, Nelson says. "The more virus in the blood, the more damage it can do to the body," he explains, listing off the risks of heart attack and stroke as just a few concerns. Plus, he points out, taking medications to suppress HIV prevents people from spreading the virus to others.
RELATED: Billy Porter Is HIV Positive—Here's What That Means and Why He's Going Public 14 Years Later
What might this news mean for the future of HIV treatment?
For now, it's important for patients who are diagnosed with HIV to undergo the recommended treatment, Dr. Adalja says. "This [case example] is an elite controller, did not really involve any anti-retroviral treatment, and cannot be easily extrapolated to the general HIV population," he says.
Turk agrees. "When most people living with HIV stop their treatment, the viral load—amount of virus in the blood—bounces from undetectable to detectable levels," she explains. "This reflects that the virus is still in the body, hidden, but ready and able to replicate. In other words, the cells in most people contain 'competent' viruses."
But Dr. Yu is optimistic that things may change in the future. "A cure of HIV is possible and can happen spontaneously in rare cases," she says.
"It may be possible in the future to develop immune interventions that lead to a cure of HIV," Dr. Laufer agrees. "If we are able to understand how her immune system reached this effect, then there might be a chance to generate a therapy to recapitulate to same effect in every person living with HIV. Still, we must say that there is still a long way to go. Current treatments, although not curative, are the best tool we have nowadays to control de virus and remain healthy."
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>The 51-year-old revealed that he was diagnosed with HIV more than a decade ago but hid it from castmates, collaborators, and even his own mother, the publication reported.
 Billy Porter HIV and filed for bankruptcy earlier that year. By June, he learned that he was HIV-positive. "The shame of that time compounded with the shame that had already [accumulated] in my life silenced me, and I have lived with that shame in silence for 14 years," Porter confessed in the interview. "HIV-positive, where I come from, growing up in the Pentecostal church with a very religious family, is God's punishment."
Billy Porter HIV and filed for bankruptcy earlier that year. By June, he learned that he was HIV-positive. "The shame of that time compounded with the shame that had already [accumulated] in my life silenced me, and I have lived with that shame in silence for 14 years," Porter confessed in the interview. "HIV-positive, where I come from, growing up in the Pentecostal church with a very religious family, is God's punishment."
Playing Pray Tell, his HIV-positive character in Pose, gave him an opportunity "to say everything I wanted to say through a surrogate," he said.
Porter described coming to terms with his truth while sheltering with his husband in a house on Long Island. COVID "created a safe space" to reflect on the trauma in his life, which includes being sexually abused as a child and coming out at age 16 in the midst of the AIDS crisis.
He's since come clean to his mother who reportedly scolded, "You've been carrying this around for 14 years? Don't every do this again. I'm your mother, I love you no matter what."
RELATED: This 29-Year-Old Went to the Doctor for a Rash—and It Turned Out He Had HIV
What does it mean to be HIV positive?
While there's still no cure for HIV, there are very effective treatments that allow people to live healthy lives and protect their partners from infection, says the US Centers for Disease Control and Prevention (CDC). HIV is now considered a chronic condition.
In the US, HIV is mainly spread through anal or vaginal sex, or sharing needles, syringes, or other drug injection equipment, per the CDC. The virus can be transmitted through semen, vaginal fluid, or blood. While anal sex poses the greatest risk of infection, women mostly get it through vaginal sex. The virus can enter the body through the mucous membranes of the vagina and cervix, CDC notes.
How do you know if you have HIV?
While HIV may cause flu-like symptoms during the first two to four weeks after infection, the only way to truly know if you've been infected is to get tested. A simple blood test or cheek swab can detect the infection. If it's positive, follow-up testing is needed to confirm the diagnosis.
It's recommended that everyone 13 to 64 get tested for HIV at least once, but frequent testing is important for anyone at risk. That includes men who have sex with men, people who inject illicit drugs or share needles, and anyone with multiple sex partners.
RELATED: 16 HIV Symptoms Every Woman Should Know
How is HIV treated?
Anyone diagnosed with HIV should begin taking HIV medications, called antiretroviral therapy, right away to reduce the amount of HIV in the body (aka your "viral load), according to the CDC. When taken as directed, these medicines can suppress that viral load in a person's body to an undetectable level, which keeps the immune system humming along. It also prevents the spread of HIV to a partner through sex.
There are also medicines that people at high risk of contracting HIV can take to prevent infection, called pre-exposure prophylaxis (PrEP). There are also drugs that can stop HIV in its tracks after a single, high-risk exposure, so-called post-exposure prophylaxis (PEP), but they have to be taken immediately after exposure. PEP doesn't replace other preventive measures. It's not intended for routine use; it's given in emergency situations, per the US Department of Health and Human Services (HHS). It's typically given to health care workers and first responders who may have been exposed to the infection through blood or other body fluids, say, through a needlestick injury, HHS points out.
To prevent HIV infection in the first place, using a condom every time you have sex will slash your chances of getting infected, per the CDC.
RELATED: 10 Things You Never Knew About HIV and AIDS
As for Porter, he feels that he survived HIV and the trauma in his life so that he could tell his story.
"The truth is healing," he said. "I hope this frees me so that I can experience real, unadulterated joy, so that I can experience peace, so that I can experience intimacy, so that I can have sex without shame."
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>That's the warning coming from the New Mexico Department of Health, who are urging customers of the VIP Spa, in Albuquerque, to consider getting tested for HIV after two clients tested positive for HIV.
"NMDOH is investigating two cases of HIV infection among VIP Spa clients who received injection-related procedures at the VIP Spa between May and September 2018," a statement from the NMDOH says.
Health officials are specifically encouraging people who received a vampire facial at the establishment to get tested for HIV. The two clients who are HIV positive also have the same HIV virus type, which increases the likelihood that the infections are the result of a procedure at the spa they both went to.
"While over 100 VIP Spa clients have already been tested, NMDOH is reaching out to ensure that testing and counseling services are available for individuals who received injection-related services at the VIP Spa. Testing is important for everyone as there are effective treatments for HIV and many hepatitis infections," Kathy Kunkel, cabinet secretary at the NMDOH, said in the statement.
You might be wondering how an unsuspecting person getting a facial at a spa could end up with a blood-borne infection like HIV. First, you need to understand exactly what a vampire facial is.
When you get a vampire facial, small amounts of blood—your blood, that is—are injected into the skin of your face. Other names for the facials are PRP facials (platelet-rich plasma facials) or PRP injections. Kim Kardashian famously posted a photo of herself trying one in 2013.
The treatment seems a little extreme, but it might be helpful to your skin, according to Bruce E. Katz, MD, a New York City-based dermatologist. "[The PRP] stimulates collagen, new blood supply and vessels, and even hair follicles," Dr. Katz previously told Health.
RELATED: A Facial That Went Horribly Wrong Left Our Beauty Director With Raw Skin for Days
Dr. Katz isn't the only physician who believes PRP facials have benefits. "PRP can be combined with microneedling to improve large pores, acne scars, and fine lines," Debra Jaliman, MD, another New York City-based dermatologist, previously told Health.
If having your own blood injected into your face sounds appealing, make sure you pick the right place to try the treatment. "Any persons desiring cosmetic services involving needle injections should verify the services are being provided by a licensed medical provider," warns the NMDOH statement.
The VIP Spa was closed in September of last year, according to the statement, after inspectors, "identified practices [there] that could potentially spread blood-borne infections, such as HIV, hepatitis B, and hepatitis C to clients."
That said, trying a vampire facial might be worth your while if you're stressing over your skin. But make sure you book an appointment only with trusted, licensed professionals when a treatment calls for needle infections in your face.
RELATED: This Video of Ashley Graham Getting an Acupuncture Facial Is the Best Thing You’ll See Today
]]>A person known only as the "London patient" has been free of the HIV virus for more than a year since receiving a bone marrow transplant from a donor who had a specific gene mutation that prevented HIV from taking hold. Researchers reported the case in the journal Nature and at this week's Conference on Retroviruses and Opportunistic Infections in Seattle.
While the investigators are calling this a "long-term remission" rather than a "cure," others are using the C word.
The only other time a patient was "cured" of HIV/AIDS was 12 years ago, in 2007. The "Berlin patient," aka Timothy Ray Brown, now 52 and living in Palm Springs, California, is widely considered cured because he has been HIV-free without anti-HIV drugs for more than a decade.
RELATED: 10 Things You Never Knew About HIV and AIDS
"The concept of a cure for HIV is really being able to remove the virus," David Rosenthal, DO, PhD, medical director of the Center for Young Adult, Adolescent, and Pediatric HIV at Northwell Health in Great Neck, New York, who was not involved in the London patient's care, tells Health. "For hepatitis C, we can completely cure people of the virus so they're no longer infected. HIV is like high blood pressure; we can control the symptoms, but we can't remove the cause."
The holy grail of HIV/AIDS research has been to rid the body of the virus permanently.
The Berlin patient's cure was one of magnificent serendipity. He underwent a bone marrow transplant to treat not AIDS but leukemia. Bone marrow transplants have long been used to treat this type of blood cancer. The bone marrow donor turned out to have a mutation that prevented HIV from digging in. The donated cells, with their ability to fight HIV, have now taken root in Brown's body.
"What we're talking about with a bone marrow transplant is getting rid of someone's immune system and giving them back someone else's immune system," says Dr. Rosenthal.
Brown, though, had terrible side effects from the treatment and nearly died. Partly for that reason, doctors have not considered this a viable option for HIV/AIDS patients.
RELATED: 16 Signs You May Have HIV
Fast forward to 2016 when the London patient received a bone marrow transplant from a donor with the same mutation. Again, the procedure was intended to treat Hodgkin's lymphoma, not HIV/AIDS. Like Brown, this patient also received immunosuppressive drugs after the transplant. The London patient stopped anti-HIV drugs more than a year ago (in September of 2017) and has had no sign of the virus since. Unlike Brown, though, the London patient did not have to go through a horrific, near-death experience to reap the benefits of the therapy.
"The question is, is it in remission, which means that we've been able to stop the virus from reproducing itself temporarily, or is it truly cured, in which case it won't ever come back?" says Dr. Rosenthal. The London patient has been free of the virus for a substantial amount of time, he acknowledges, but at this point, "it's still possible for the virus to come back."
Today, people with HIV are able to live essentially virus-free with a minimally disruptive regimen of pills.
"Medications used to be much more difficult and have higher side effects," says Dr. Rosenthal. "We're fortunate now in that we can have many patients treated with one pill, once a day. That completely suppresses the virus [making it] undetectable." That may sound like a cure but it's not: When the medications stop, the virus comes back.
So does the case of the London patient mean we're on the verge of having a widely available cure for HIV/AIDS? Not so fast.
"We really don't know what the long-standing significance of this is," says Dr. Rosenthal. "We can't completely eradicate everyone's immune systems and this, in and of itself, is not a suggested mechanism for curing HIV." Bone marrow transplant procedures are rough, involving heavy-duty drugs, serious side effects, and the possibility of death.
But the current news "does teach us a great deal about the HIV virus and how we can possibly create other ways to eradicate it," says Dr. Rosenthal. "I don't think doing wide-scale bone marrow transplantation is on anyone's radar as a future option."
RELATED: This 29-Year-Old Went to the Doctor for a Rash—and It Turned Out He Had HIV
Researchers are tracking other HIV/AIDS patients who have received bone marrow transplants from donors with the same mutation that cured the Berlin patient. "Patients are being monitored to see how well they do and how well they continue to do,” says Dr. Rosenthal. "If you don't have any virus that can be detected for an extended period of time, when does that become a cure instead of remission?"
Both the London patient and those currently being monitored, he adds, “help us understand how we can overcome the virus and design a true cure.”
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>The risk of infection is low, the state's Department of Health told Reuters last week, but today, CNN reports that a 58-year-old, unidentified Brooklyn woman has tested positive for hepatitis B after having shoulder surgery at HealthPlus Surgery Center. The medical center told all 3,778 patients who were affected by the lapses in protocol to get blood tests “out of an abundance of caution” and that it would pay for all testing.
It’s hard to imagine how scary it must be to receive a letter—let alone a diagnosis—like that, and even though this incident doesn’t involve the vast majority of us, it’s gone viral online and made headlines around the country. For starters, viruses like HIV and hepatitis are serious stuff. But also, it feels like something that could happen to pretty much anyone in the wrong place at the wrong time.
That’s why we thought this would be a good time for a refresher on how, exactly, HIV and hepatitis can—and can’t—be transmitted from person to person, and what to do if you think you may have been exposed. Health spoke with Stuart Ray, MD, professor of medicine and infectious disease specialist at Johns Hopkins University School of Medicine, to get his thoughts and advice.
RELATED: 16 Signs You May Have HIV
This kind of thing happens rarely—but not never
First things first, says Dr. Ray: This news shouldn’t scare anyone off from visiting the doctor or having necessary medical procedures done. Federal and state health departments both have standard precautions in place to keep medical equipment sterilized and cared for properly, he says, “and when those steps are followed, the risk of infection is very, very low.”
However, he says, this isn’t the first time something like this has happened. In 2004, 16 people were infected with hepatitis after undergoing cardiac stress tests at clinics in Maryland; it was later revealed that the dye injected into their veins was contaminated.
Between 2008 and 2017, the CDC has recorded 61 outbreaks of viral hepatitis related to health care. (Many of those cases involved health care workers, who are at much higher risk than patients.) As for the HIV transmission in a health care setting, the CDC says it’s possible but “extremely rare.”
“These things happen from time to time, and they’re a risk that goes along with any percutaneous procedure, anything that punctures the skin,” says Dr. Ray. That being said, millions of Americans get these procedures every year with no ill effects whatsoever.
The risk of infection is (usually) extremely low
Even if you are exposed to a virus like HIV or hepatitis via an infected person’s blood, there’s still a good chance you won’t become infected, says Dr. Ray. Say you were stuck with a needle that contained an infected person’s blood, for example: Your risk of getting hepatitis B, hepatitis C, or HIV is approximately 1 in 3, 1 in 30, and 1 in 300, respectively.
“A big reason for this variability in transmission is because the levels of the virus in the blood vary, and they tend to be highest for hepatitis B and lowest for HIV, even when someone has a high level of infection,” says Dr. Ray. “So even though HIV is not curable, fortunately it has the much lower transmission rate.”
The other important thing to remember is that hepatitis and HIV are only transmitted through blood or sexual contact—so you can’t get infected just by being in the same hospital or doctor’s office as someone with these diseases.
There are treatments for hepatitis
Many people who are exposed to hepatitis B will never get infected, thanks to a vaccine that’s now recommended for all children, health care workers, and other adults at higher than average risk. And if an unvaccinated person is infected with hepatitis B through a medical error, antiviral medications can help keep the disease under control.
There’s no vaccine for hepatitis C, but the risk of transmission is also significantly lower than it is for hepatitis B. Additionally, about one in three people who are infected with hepatitis C will clear the infection on their own.
“Even for those cases that don’t clear up on their own, we can cure them with a treatment that takes about eight to 12 weeks,” says Dr. Ray. “That’s a big advance: It means that the number one cause of liver failure in the United States can now be cured.”
RELATED: Pamela Anderson Cured of Hepatitis C
And there are prophylactic treatments for HIV
There is no cure for HIV, but there are medications—known as pre-exposure prophylaxis, or PrEP—that can reduce the risk of transmission if taken shortly before or after HIV exposure. These drugs are sometimes taken by people who have HIV-positive sex partners, but they can also be taken after accidental exposure.
Of course, if someone only found out weeks or months later that they’d been exposed to HIV, this type of treatment wouldn’t be helpful. Even if exposure is caught right away, these drugs are expensive and can have serious side effects—so “we recommend them sometimes, but only when the risk of infection is higher than the risk of the prophylaxis,” says Dr. Ray.
Health care facilities aren’t the only place you could be exposed
The New Jersey surgery center in the news has cast a spotlight on hospitals and doctors' offices, but people can be exposed to potential infections outside of medical settings as well. Earlier this year, clients of a New Mexico spa were told to get tested for HIV and hepatitis after one person reported an infection after undergoing a vampire facial, a procedure that draws blood and then reinserts it into the face.
There are also more than 3 billion medical injections made outside of health care facilities every year, according to SafeNeedleDisposal.org—and those needles, syringes, and other “sharps” devices could put others at risk if they’re not disposed of safely. And as the opioid epidemic rages across the United States, it’s also not unheard of for people to encounter syringes used for illicit drug injections in bathrooms, parks, and other public places.
Fortunately, there has never been a reported case of HIV transmission through a “community found syringe accidental needle stick,” according to the Indiana Recovery Alliance—and the risk of acquiring a hepatitis infection in this way is “practically negligible.”
Still, it’s important to know how to dispose of a syringe if you do find one. Your safest bet? Contact your local police or health department; they should have the equipment necessary to handle the device without putting anyone else at risk.
RELATED: 8 Things You Didn't Know About Hepatitis
What to do if you think you’ve been exposed
If your skin is punctured by an unsterilized needle—in a health care setting or anywhere else—Dr. Ray suggests first washing the injection site thoroughly with water and soap or a sterile solution if one is available. “Don’t use bleach or aggressive chemicals, and don’t try to squeeze it to milk out the poison,” he says. “That can actually do more harm than good, since it can injure the tissue and make it more vulnerable.”
Then call your doctor or a hospital for advice on what to do next. If the puncture actually caused you to bleed, or if it’s suspected that someone who previously used the needle has a transmittable virus, you may be encouraged to get prophylactic treatment or undergo testing.
For people involved in a large protocol lapse like the one in New Jersey, Dr. Ray recommends that every patient who had blood work or injections during the affected time period get tested. As a letter sent to HealthPlus patients points out, “you can be infected with these diseases and not feel sick at all.”
The good news, says Dr. Ray, is that announcements like the one from the New Jersey clinic usually are truly out of an abundance of caution and that even people who were directly involved should not assume the worst. “In almost all of these cases, the number of people actually infected is very small compared to the number of people going through the door,” he says.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>A 29-year-old man went to a dermatology clinic complaining of an itchy, inflamed, and scaly rash on his back—and you can see the alarming photos in today’s issue of the New England Journal of Medicine. The authors note that he had had the rash two years earlier but hadn’t gone to see a doctor until now.
The first thing doctors do is take a patient’s medical history, in order to begin to go down the right path for a potential diagnosis. This patient suffered from eczema as a child, as well as seasonal allergies. Certain medications can cause rashes, but, as the authors note, he wasn’t taking anything.
Next up was a physical exam. More than 90% of his body had an inflamed, violet-hued plaque (a patch of thick, scaly skin), as shown in the photo below. On the right, an area near his shoulder blade that wasn’t affected gives you an idea of just how widespread this rash was.
 Erythrodermic Psoriasis and HIV Infection
Erythrodermic Psoriasis and HIV Infection
Generally, say the authors, these symptoms could point to possible diagnoses including erythrodermic psoriasis (an inflammatory form of psoriasis that affects most of the body, according to the National Psoriasis Foundation), seborrheic dermatitis (often affecting the scalp, causing dandruff), and pityriasis rubra pilaris (a group of rare diseases that cause red, scaly patches that spread over the whole body).
After a skin biopsy from two places on his back, the doctors landed on their diagnosis: erythrodermic psoriasis. This rare type of the skin condition only affects 3% of people with psoriasis. While the case study doesn’t mention the patient’s comfort level, the condition can be painful and very, very itchy. Along with redness, skin can shed in large “sheets.” It may also cause protein and fluid loss and affect the body’s ability to regulate its temperature—dangerous side effects that can actually be life-threatening. (And remember, this patient waited two years to seek treatment.)
RELATED: The Different Types of Psoriasis
It’s one thing to treat the rash, but often, the skin reveals a systemic disease simmering beneath the surface. Doctors look for potential underlying causes like infections, alcoholism, severe sunburns, or emotional stress. In the NEJM case, an HIV test came back positive. The patient was then given antiretroviral drugs, medications that stop the progression of HIV, and a topical corticosteroid to treat the rash itself. After three months, his skin cleared.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>World AIDS Day was first observed in 1988. The day was originally conceived by the World Health Organization to raise awareness and support. This year marks the 31st World AIDS Day, with the 2019 theme being Communities Make the Difference. That theme comes with two major objectives, according to the WHO: "highlighting the difference these communities are making to end HIV while drawing global attention to the need for broader engagement with them to strengthen primary health care."
The day is an opportunity to take stock of the epidemic's scope and the everyday impact of the virus–and what better way to do this than by reminding ourselves of the often alarming numbers involved?
The stories of individuals who have lived with HIV/AIDS, or who have lost a loved one to the illness, will always have a unique power. But the following statistics, gathered from government data and scientific research, bring home the vastness and complexity of the epidemic.
RELATED: 16 Signs You May Have HIV
|
1.1 million |
= Estimated number of HIV-positive people in the United States |
This figure works out to about 1 in every 200 people over the age of 13. What's more, 1 in 7 don't know they're infected because they haven't been tested for the virus.
Globally, an estimated 36.9 million people are living with HIV/AIDS—nearly 70% of them in Africa. While the rate in the United States may seem low by comparison, it still is one of the highest in the developed world, says Michael Horberg, MD, director of HIV/AIDS at Kaiser Permanente. (In the U.K., for instance, roughly 1 in 625 people are estimated to be HIV-positive.)
RELATED: What Is HIV?
|
12,333 |
= Estimated annual U.S. deaths from HIV/AIDS |
This statistic, from 2014 (the most recent year for which solid data is available), is heartbreaking yet also encouraging: It's about a quarter of the number of people who died of HIV/AIDS in 1995, when mortality reached an all-time high and dramatically less than the 21,601 estimated deaths from HIV/AIDS in 2009.
The sharp decrease is a testament to improved testing, diagnosis, and treatment. "This number, while still too high, shows that quality HIV care, and the potent medications we now have, [have] dramatically improved the lives of HIV-positive Americans and people worldwide," Dr. Horberg says.
RELATED: Jonathan Van Ness Reveals He's HIV Positive: 'I Do Feel the Need to Talk About This'
|
8,164 |
= People ages 13 to 24 newly infected with HIV in the United States each year |
In 2016, young people accounted for one in every five new infections in the United States, according to the Centers for Disease Control and Prevention (CDC). From 2010 to 2015, HIV infections among this age group fell 24%. In 2017, 8,164 teens and young adults between 13 and 24 were diagnosed, according to the CDC.
Unfortunately, only 10% of high school students and just 21% of male students who are sexually active with other males have been tested, according to the CDC.
RELATED: A Second Patient Has Been Cured of HIV—How Does That Even Happen?
|
43% |
= HIV-positive people in the United States who are African-American |
This is a startling number, given that African-Americans make up just 12% of the U.S. population. The burden of disease is even more disproportionate among 13- to 24-year-olds, an age group in which African-Americans or blacks (government agencies tend to use the terms interchangeably) account for 54% of new infections.
"HIV is now a disease of minorities—black, Latino, gay men—and people who have been often medically disenfranchised in the past," says Dr. Horberg, who is also chair of the HIV Medicine Association, a professional association for doctors and health care providers who specialize in HIV/AIDS.
RELATED: This 29-Year-Old Went to the Doctor for a Rash—and It Turned Out He Had HIV
|
10 years |
= Time after HIV infection that can elapse before noticeable symptoms appear |
People can live with HIV for a decade (or longer) before they experience symptoms such as fever, fatigue, and joint pain—a fact that underscores the importance of testing and early detection.
Thanks to virus-fighting drugs (antiretrovirals), this asymptomatic period, known as the "chronic" or "latency" phase of the disease, can essentially be extended indefinitely. "If people are diagnosed early and given effective treatment, and if they stay on their treatment, they won't have any symptoms at all," Dr. Horberg says.
RELATED: Woman, 45, Who Was Diagnosed with HIV at 18, Shares Her Powerful Story: 'I Believe in Life'
|
46% |
= U.S. adults ages 18 to 64 who have never been tested for HIV |
The number of people getting tested for HIV rose between 1997 and 2004 but has leveled off since then, according to the 2014 Kaiser Family Foundation survey results that produced the above statistic. Black and Latino survey respondents were much more likely than whites to report having been tested.
In the United States, National HIV Testing Day is observed on June 27, but World AIDS Day also features free testing and counseling events around the world.
|
13 to 64 |
= Age range for which routine HIV testing is recommended |
The CDC recommends that everyone between these ages get tested for HIV at least once. People considered at higher risk for HIV should get tested more frequently, according to CDC guidelines.
Routine screening helps get more people into treatment sooner, Dr. Horberg says. "Not only does treatment help patients, but it will also greatly prevent others from getting infected."
RELATED: How to Prevent HIV
|
75% |
= Proportion by which antiretroviral drugs can reduce the risk of HIV transmission |
The antiretroviral Truvada became the first drug approved by the Food and Drug Administration for preventing the sexual transmission of HIV in 2012. In one study of heterosexual African couples in which one partner was HIV-positive, the HIV-negative partners who took Truvada had a 75% lower risk of becoming infected compared with those taking placebo.
There are a number of caveats—most notably, people must diligently take the drug every day in order for it to be effective. But the study results do "show that there are many effective ways to prevent HIV infection," Dr. Horberg says. In 2017, 21.7 million people living with HIV were taking antiretroviral therapy, according to UNAIDS.
RELATED: Child With HIV Has Been in Remission For Nearly 9 Years Without Drugs
|
16% |
= Drop in new HIV infections between 2010 and 2017 |
This decline is among the many bright spots in the World AIDS Day 2018 fact sheet from UNAIDS. In some regions hit hardest by the epidemic, the numbers are even more encouraging: From 2010 to 2016, new infections dropped by 29% in eastern and southern Africa.
RELATED: Drug-Resistant HIV Is On the Rise
|
$21.3 billion |
= |
Money spent on HIV/AIDS efforts in low- to middle-income countries each year |
This includes donations from governments, corporations, and individuals. Although the amount represents a huge increase from the $300 million spent in 1996, even more is needed: UNAIDS estimates $26.2 billion will be required to maintain these efforts in 2020.
Fighting HIV/AIDS is expensive. But in addition to saving lives, the investment will ultimately drive down worldwide health care costs, Dr. Horberg says. "There will be savings down the line, because you will have fewer newly infected people, people will be generally healthier, [and] they won't be hospitalized," he says.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
What is HIV?
HIV can affect anyone, but gay and bisexual men are particularly vulnerable, accounting for more than two-thirds of all newly diagnosed cases in the U.S. Black and Hispanic people are disproportionately affected.
HIV is commonly transmitted through sexual contact or use of shared needles, syringes, or other materials used for injecting drugs. There’s no cure for HIV, but medications can keep the infection from worsening.
What is AIDS?
AIDS, short for acquired immunodeficiency syndrome, is the most advanced stage of HIV. It refers to the set of symptoms a person develops when the immune system is too weak to fight off infection.
People with AIDS have severe immune-system damage. This can be determined two ways. One is by the number of CD4 cells in a sample of blood. (A CD4 cell is a type of white blood cell that attacks infection.) HIV destroys CD4 cells, so a person’s count declines. AIDS is diagnosed when the CD4 count falls below 200 cells per cubic millimeter of blood. (A healthy person has a count of between 500 and 1,500.) Another sign of AIDS is when the person infected with HIV develops one or more infections, regardless of their CD4 count, that are more common or more severe among people with weakened immune systems. These infections are called opportunistic infections.
Without treatment, HIV gradually destroys the immune system. The time it takes for HIV to progress and become AIDS varies from person to person. On average, it takes 10 years. Advances in treatment have helped millions stave off symptoms of AIDS.
RELATED: 20 Things You Need to Know About HIV
Signs and symptoms of HIV
HIV symptoms are not a reliable indicator of infection. Some people may feel sick within the first four weeks of infection, while others may show no symptoms for 10 years or more. Plus, the early signs of HIV are much like any other infection. So the only way to know whether you have it is to get tested.
An estimated 40 to 90% of people with HIV experience flu-like symptoms within two to four weeks of being infected, according to the U.S. Centers for Disease Control and Prevention (CDC). Some people may not feel sick at all in the early stage of HIV, also known as acute infection. HIV may not even show up on some diagnostic tests at this early stage. Yet this is the time when the virus is most contagious.
Early symptoms of HIV, meaning signs that occur within the first six months of infection (including the first two to four weeks) may include fever, muscle aches, fatigue, swollen lymph nodes, or some combination of flu-like symptoms. HIV rash can be a symptom of infection or a side effect of medication.
Symptoms may last a few days to a few weeks and can include:
- Fever
- Chills
- Sore throat
- Mouth ulcers
- Headache
- Rash
- Night sweats
- Fatigue
- Muscle aches
- Diarrhea
- Swollen lymph nodes
After the early stage of infection, people with HIV may have mild or no symptoms. Even without treatment, this chronic stage of the disease can last for a decade, while people taking medications for their HIV can live in this stage even longer. However, the virus remains active and HIV is still contagious at this stage. Even people who don’t have symptoms can transmit the infection to others. Treatment reduces the amount of virus in the blood, making transmission less likely.
Without treatment, HIV eventually batters the immune system to the point that people living with this infection are prone to all sorts of serious illnesses. Late-stage HIV symptoms may include:
- Rapid weight loss
- Recurring fever
- Extreme fatigue
- Persistent cough
- Mouth, anus, and/or genital sores
- Swollen lymph glands in the armpits, groin, and/or neck
- Memory loss, depression, or other neurologic issues
- Chronic diarrhea
- Blotchy skin
- Pneumonia
- Night sweats
RELATED: 16 Signs You May Have HIV
What causes HIV?
HIV attacks and kills a specific type of white blood cell, called a CD4 cell. Normally, these cells guard against infection. But, when HIV enters the bloodstream, the virus uses these cells to makes copies of itself and spread throughout the body.
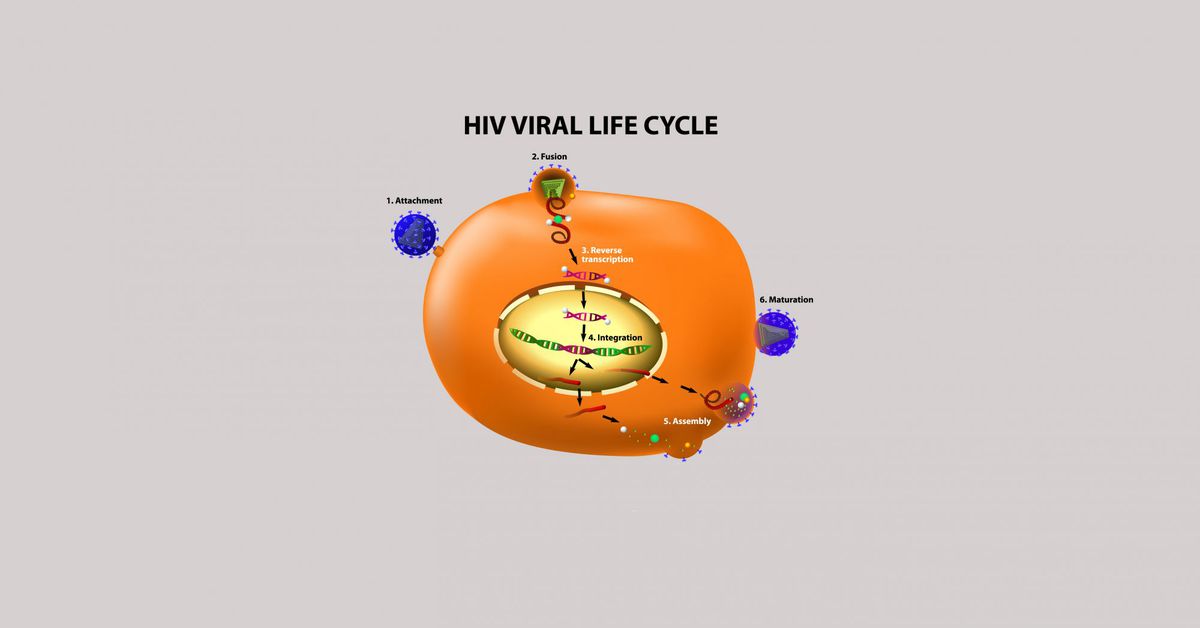
The process takes place over several stages, known as the “HIV life cycle.” First, HIV binds to the surface of the CD4 cell and then fuses with the cell membrane to enter the cell. From there, it converts its genetic material (RNA) into DNA, allowing the virus to enter the cell nucleus. There, HIV inserts its viral DNA into the DNA of the CD4 cell and produces HIV proteins that can be used to make more HIV. Finally, those new proteins and new HIV RNA are pushed out of the cell, forming new HIV capable of infecting other cells, and the process begins all over again.
HIV is believed to have existed in the U.S. since the 1970s. Scientists trace its roots to Central Africa. They believe a virus found in chimpanzees jumped species and mutated into HIV sometime in the late 1800s, when humans hunting chimps for meat were exposed to the animals’ blood. U.S. health officials reported the first case of what later became known as AIDS in June 1981.
 condom stuck in vagina what to do HIV is not acquired through casual contact. You don’t get it from saliva or tears, kissing, mosquito bites, shared toilet seats, or food prepared by someone with HIV. (Open-mouth kissing may be risky if both partners have mouth sores or bleeding gums.) And while HIV used to be passed through donated blood, organs, and tissues, screening procedures in the U.S. have dramatically lowered that risk.
condom stuck in vagina what to do HIV is not acquired through casual contact. You don’t get it from saliva or tears, kissing, mosquito bites, shared toilet seats, or food prepared by someone with HIV. (Open-mouth kissing may be risky if both partners have mouth sores or bleeding gums.) And while HIV used to be passed through donated blood, organs, and tissues, screening procedures in the U.S. have dramatically lowered that risk.
HIV prevention
People can avoid getting HIV and lower the chances of infecting other people with the virus by taking advantage of multiple prevention strategies.
The most effective way to prevent the transmission of HIV from person to person is to abstain from anal, vaginal, and oral sex.
Before having sex, know your partner’s HIV status or talk to your partner about getting tested for HIV. You and your sex partner also should be tested for other sexually transmitted diseases (STDs) and receive treatment if necessary. Having an STD can increase the risk of getting HIV and passing the virus to others.
Using condoms correctly every time you have any kind of sex (vaginal, anal, or oral) is crucial. Condoms provide a barrier that can provide protection from HIV. If you are HIV-positive, using a condom can reduce the risk that you will transmit the virus to others.
If you are HIV-negative, having fewer sex partners can lower your risk of having a partner with HIV or another STD. And, if you are at high risk of acquiring HIV, talk to your doctor about taking daily medicine called pre-exposure prophylaxis to prevent infection.
If you think you’ve been exposed to HIV, seek immediate medical care. Starting medicines called post-exposure prophylaxis within 72 hours of exposure can help prevent infection.
If you are HIV-positive, you can protect your partner and yourself by taking antiretroviral therapy–medicines that reduce the amount of HIV in your blood and body.
RELATED: How to Prevent HIV
HIV pictures
HIV infection is immediate but the impact on a person’s immune system evolves over time.
Within a couple of weeks of getting HIV, you may experience flu-like symptoms, like fever and fatigue. During this acute stage, the virus multiplies rapidly and spreads throughout the body.
Eventually, HIV enters a chronic stage. The virus remains active but replicates at a slower rate. You may feel better and have fewer or no symptoms. But the virus will eventually wreck your immune system if you don’t seek treatment.
The final stage is full-blown AIDS. This occurs when the number of infection-fighting white blood cells, called CD4 cells, declines, and/or when you develop at least one additional serious infection or disease.
Bacterial, fungal, viral, and parasitic infections, including pneumocystis pneumonia, Kaposi’s sarcoma (a type of cancer that causes spots on the skin), and tuberculosis are called opportunistic infections. These infections take advantage of a person’s damaged immune system.
Opportunistic infections are less common today than at the height of the AIDS epidemic because new treatments enable people with HIV to live longer, healthier lives. But they can still occur, especially if people don’t know they have HIV or don’t seek treatment.
 GettyImages-509233595 Fingernail and toenail changes can happen to anyone but are more common in people with compromised immune systems. People with HIV and AIDS commonly develop onychomycosis, a fungal infection that causes nails to discolor, thicken, and separate from the nail bed.
GettyImages-509233595 Fingernail and toenail changes can happen to anyone but are more common in people with compromised immune systems. People with HIV and AIDS commonly develop onychomycosis, a fungal infection that causes nails to discolor, thicken, and separate from the nail bed.
How is HIV diagnosed?
One in seven people in the U.S. have HIV but don’t know it. The only way to confirm a diagnosis is to get tested.
Most HIV tests (including test kits for home use) detect antibodies that your body produces in response to the virus. “Rapid” antibody screening tests can provide results in 30 minutes or less. These tests use blood or a swab of your mouth. Most people develop antibodies within three to 12 weeks of being infected.
Combination HIV tests use blood to look for antibodies that your body makes as well as antigens–or proteins–that are part of the virus. It takes two to six weeks for someone with HIV to make enough antibodies and antigens for this test to detect the virus. These tests are becoming more common in the U.S.
Nucleic acid tests detect the infection in blood, but they are expensive and not routinely administered unless someone has had a high-risk exposure to HIV or possible exposure with early HIV symptoms.
No test can immediately detect the virus. There’s a window of time between exposure to the virus and when these tests can reliably detect HIV. But you should talk to your doctor immediately if you think you may have been exposed to HIV.
Positive results must be confirmed with further testing before a diagnosis is made. A negative result within three months of exposure should be repeated three months later.
RELATED: 7 Myths About HIV
HIV treatment
HIV treatment is called antiretroviral therapy (ART), which involves taking a combination of medicines every day. More than 25 medicines are approved by the U.S. Food and Drug Administration (FDA) to treat HIV, and some of these medicines are available as combination pills.
These medicines fall into six drug classes that differ in how they attack the virus. Each class of medicines targets the virus at a different stage of the HIV life cycle.
ART doesn’t cure HIV. But it does slow the virus’s attack on the immune system, keeping people healthier longer. It also helps reduce the risk of HIV transmission. The U.S. Department of Health and Human Services (HHS) recommends that people diagnosed with HIV start antiretroviral therapy immediately.
The specific medicines in each person’s HIV drug regimen vary depending on individual needs, including the amount of virus in a person’s blood, other health conditions a patient may have, or whether she is pregnant. Doctors may also consider possible side effects and potential drug interactions as well as the cost and convenience of various options when prescribing ART.
Typically, it takes three to six months for these medicines to reduce the amount of virus in the blood to an undetectable level.
 GettyImages-522930436 Other medicines. These include cobicistat, a drug used to boost the effectiveness of an HIV medicine, and more than a dozen products that combine two or more HIV medicines from different drug classes.
GettyImages-522930436 Other medicines. These include cobicistat, a drug used to boost the effectiveness of an HIV medicine, and more than a dozen products that combine two or more HIV medicines from different drug classes.
When to see a doctor
Even if you don’t feel sick, talk to your health care provider if you think you’ve been exposed to HIV. No test can immediately detect the virus, but your doctor can advise you about when to start testing and what precautions to take. He or she may also conduct a baseline physical evaluation.
Seek immediate medical attention if you are HIV-negative (or don’t know your HIV status) and are exposed to HIV, whether it’s through unprotected sex or a condom break; needle or equipment sharing for injecting drugs; sexual assault; or, in health care settings, an accidental needlestick injury. You have 72 hours from the time of exposure to begin taking medicines (called post-exposure prophylaxis) to prevent HIV–and the sooner you start, the better.
If you test positive using a home test kit, see your doctor or find an HIV specialty clinic that can provide follow-up testing and ongoing care. In fact, any positive test requires a confirmation.
People who are HIV-positive can expect to have repeated lab tests as part of their routine care and more frequent visits anytime there is a change in symptoms or medications. Ongoing care may also require visits with a range of health care providers–including dentists, counselors, and other medical specialists–to manage the condition.
RELATED: 10 Questions to Ask a New Partner Before Having Sex
Is HIV curable?
There’s no cure for HIV, but it’s manageable if patients take their medicines as directed. People who are treated before the disease progresses too far can expect to live nearly as long as someone who does not have HIV, according to the CDC.
Antiretroviral drugs introduced in the mid-1990s prolong life by reducing a person’s “viral load”–the amount of virus in the blood and body fluids–and boosting their CD4 (white blood cell) counts. That gives the immune system a fighting chance.
Taking these medicines regularly, as directed, can prevent HIV-related opportunistic infections and lower your risk of infecting other people. While HIV remains present in blood and body fluids, the amount of virus declines, ideally to an undetectable level. That’s why it’s important to get diagnosed as soon as possible to initiate treatment.
The decades-long search for a vaccine to prevent HIV infection or treat people who are HIV-positive continues. According to HIV.gov, an official website of the HHS, even a vaccine that only protects some people would go a long way toward reducing the number of new HIV infections.
 GettyImages-587169665 can progress more quickly than in adults, according to the CDC. But, the earlier a child with HIV starts taking antiretroviral treatment, the better off he or she will be.
GettyImages-587169665 can progress more quickly than in adults, according to the CDC. But, the earlier a child with HIV starts taking antiretroviral treatment, the better off he or she will be.
Often, these infections occur during childbirth. Treating the mother can prevent the transmission of HIV to her baby. Plus, a short course of HIV medicine for the baby can provide added protection. These children typically receive zidovudine for four to six weeks after birth.
Breast milk also poses a risk if a new mom is HIV-positive. The HHS recommends that HIV-positive women use infant formula instead.
Testing babies for HIV usually begins at 14 to 21 days after birth and continues at one to two months and again at four to six months. Two negative or two positive tests are required to confirm his or her HIV status.
Thanks to preventive measures, there has been a dramatic reduction in the number of babies born with HIV in the U.S. The estimated number of infants born with perinatal HIV infection (the result of mother-to-child transmission) dropped to 69 in 2013 from 216 in 2002, according to a study published in JAMA Pediatrics in 2017.
However, gaps in diagnosis and treatment remain. During the study period, a majority of moms who gave birth to infants born with HIV were black or Hispanic, and more than a third of the births occurred in just five states (Florida, Texas, Georgia, Louisiana, and Maryland).
Living with HIV
Living with HIV means sticking to a treatment plan. But life can sometimes make that difficult.
Remembering to take your medicines daily, without fail, is just one of the challenges you may face. Some medication regimens are complex, with multiple medicines taken at different times, with or without food. If you’re working or traveling, popping pills may prove inconvenient. Setting a schedule, planning ahead, and using pillboxes and other reminders may help.
HIV-related infections can make it difficult for some people to swallow pills. Talk to your health care provider about liquid versions of antiretroviral medicines or whether the pills you take can be split or crushed.
Maintaining a healthy diet is key to supporting your immune system. But that can be hard to do when you’re struggling with HIV-related metabolism changes or medication side effects, such as nausea or diarrhea. You may find it helpful to consult with a nutritionist to navigate these issues.
People with HIV may also experience mental health issues, such as depression, anxiety, and suicidal thoughts. Your doctor can help you find a qualified mental health professional. You may also benefit from finding a case manager who can help with day-to-day challenges of living life with HIV, including housing, transportation, and childcare.
RELATED: Here’s Why Some People Go Off Their HIV Meds
 Vial of blood after blood test ? If so, you should be tested for HIV as soon as possible. Women who are HIV-positive and pregnant not only have to take care of their own health, they need to preserve the health of their unborn babies.
Vial of blood after blood test ? If so, you should be tested for HIV as soon as possible. Women who are HIV-positive and pregnant not only have to take care of their own health, they need to preserve the health of their unborn babies.
Most antiretroviral medicines are safe for use during pregnancy. These medicines lower the amount of virus in the woman’s body, keeping her healthy and reducing the risk of transmitting the virus to her fetus.
If a woman is already taking HIV medicines, typically her doctor will keep her on those medicines. Any woman who learns she is HIV-positive during pregnancy should start an antiretroviral regimen as soon as possible.
A woman’s risk of transmitting the infection is greatest during childbirth, when the newborn is exposed to her blood and other body fluids. If the amount of virus in the woman’s body is high or unknown near the time of delivery, doctors typically order an IV of zidovudine, which passes across the placenta from a mom to her unborn baby. This drug prevents the mother-to-be from transmitting HIV to the baby during delivery.
A scheduled Cesarean section may be another option for reducing the risk of transmission.
Celebrities with HIV
HIV doesn’t care if you’re famous or not. Actors, athletes, and entertainers are just as vulnerable as other people who are exposed to the virus.
Los Angeles Lakers point guard Magic Johnson stunned the world with his 1991 retirement from basketball after learning he had HIV. He created the Magic Johnson Foundation to fight HIV and, decades later, remains an advocate for HIV and AIDS prevention.
Olympic diver Greg Louganis, diagnosed in 1988, has gone through many treatments throughout the years. As he told ESPN The Magazine in 2016, “HIV has taught me that I’m a lot stronger then I ever believed I was.”
Charlie Sheen publicly revealed his HIV status in 2015. In 2016, the Golden Globe-winning actor joined a clinical trial of an injectable drug called PRO 140. The experimental medication belongs to a new class of medications called entry inhibitors designed to protect healthy cells from HIV infection. Sheen reportedly credits the antiviral therapy with a positive transformation of his health, even though it is not yet FDA-approved.
Unfortunately, advances in HIV and AIDS research came too late for many celebrities, including tennis great Arthur Ashe, who believed he contracted the virus via a blood transfusion and became an advocate for public awareness of the disease.
Others who have died from HIV and AIDS include Queen’s lead vocalist and songwriter Freddie Mercury; heartthrob actor Rock Hudson; Anthony Perkins, who played Norman Bates in the psychological thriller Psycho; TV dad Robert Reed of The Brady Bunch; and Tom Fogerty, lead singer of the rock band Creedence Clearwater Revival.
]]>“I guess certain things happen for a reason,” he said. “And maybe all the stuff that I’ve done professionally, to garner such attention and fanfare and whatever else—good or bad—was sort of leading to a greater calling, a deeper calling, rather than fiction.”
Sheen, 50, told People that he has decided to partner with a condom brand called LELO HEX precisely because contraceptives are a subject people don’t like to talk about: “I figured: If I’m involved, maybe they’ll talk about it.”
RELATED: 16 Signs You May Have HIV
Safe sex can use all the publicity it can get. Despite major advances in HIV treatment, the number of people in the United States who are infected with the virus each year—about 50,000—is surprisingly high, and has remained fairly stable for the last decade. But a 2012 Kaiser Family Foundation poll found that 44% of young adults aren’t personally concerned about HIV, and another 28% aren’t “too concerned.”
What’s more, 1 in 8 people who have HIV don’t realize it, according to the Centers for Disease Control and Prevention. And as Larry Corey, MD, a principal investigator for the HIV Vaccine Trials Network at the Fred Hutchinson Cancer Research Center, pointed out in a previous interview with Health, if people don’t know they have the virus, they can transmit it to others.
“You spend five seconds putting [a condom] on, and you prevent a lifetime of stress, potentially,” Sheen said in the People interview.
RELATED: 7 Myths About HIV and the Facts You Need to Know
As for the actor’s own health, he is currently enrolled in an FDA-approved clinical trial of a new drug called PRO 140, a weekly injection he calls a “game changer” compared to traditional antiretroviral therapy: “You’re not saddled with the reminder every day: [When] you’ve gotta take your pills, you’re reminded; there’s a whole psychological aspect to that,” he said.
Sheen added that he’s excited about being a part of something “I think is going to help a lot of people.”
]]>RELATED: 20 Things You Need to Know About HIV
To reduce your risk, the National Institutes of Health recommends following these guidelines.
Use a condom every time
Seriously, every time—HIV is spread through blood, semen, pre-seminal fluids, vaginal fluids, and rectal fluids, which means that you can contract it through vaginal, oral, and anal sex. Condoms drastically reduce the risk of the virus being spread.
Get tested for HIV
Despite the fact that 45% of Americans have never gotten tested for HIV, the CDC recommends everyone between the ages of 13 and 64 be screened at least once. Those at high risk (such as IV drug users, sex workers, and anyone with an HIV-positive partner) should be tested annually. Testing is free for most people (the Affordable Care Act requires many health insurance plans to offer it without a copay) and you can get results back in just 20 minutes.
Practice safe sex
Before having sex with someone new, ask them about their sexual history. For example, have they ever tested positive for HIV or another STD? How many sex partners have they had in between those tests? Limiting the number of sexual partners you have is another way to decrease your risk.
RELATED: What to Do If Your Sex Partner Refuses to Wear a Condom
Don’t inject drugs
Because HIV can be spread by blood, sharing a needle with someone who is infected puts you at risk.
Consider a preventative treatment
Those who are at high risk of contracting HIV can reduce their odds by taking a pre-exposure prophylaxis (or PrEP). The PrEP medication Truvada is used to treat HIV and can also help prevent its spread. There are some downsides, however: Truvada is expensive (up to $14,000 a year) and can have life-threatening side effects.
]]>