Jump to: Causes | Symptoms | Diagnosis | Types | Stages | Treatment | Prevention
What is breast cancer?
Breast cancer is the most common cancer among women, after skin cancer. One in eight women in the United States (roughly 12%) will develop breast cancer in her lifetime. It is also the second leading cause of cancer death in women after lung cancer. Encouragingly, the death rate from breast cancer has declined a bit in recent years, perhaps due to greater awareness and screening for this type of cancer, as well as better treatments.
Breast cancer is a disease that occurs when cells in breast tissue change (or mutate) and keep reproducing. These abnormal cells usually cluster together to form a tumor. A tumor is cancerous (or malignant) when these abnormal cells invade other parts of the breast or when they spread (or metastasize) to other areas of the body through the bloodstream or lymphatic system, a network of vessels and nodes in the body that plays a role in fighting infection.
Breast cancer usually starts in the milk-producing glands of the breast (called lobules) or the tube-shaped ducts that carry milk from the lobules to the nipple. Less often, cancer begins in the fatty and fibrous connective tissue of the breast.
New cases of breast cancer are about 100 times more common in women than in men, but yes, men can get breast cancer too. Male breast cancer is rare, but anyone with breast tissue can develop breast cancer.
What causes breast cancer?
Breast cancer is caused by a genetic mutation in the DNA of breast cancer cells. How or why this damage occurs isn’t entirely understood. Some mutations may develop randomly over time, while others are inherited or may be the result of environmental exposures or lifestyle factors.
Most breast cancers are diagnosed in women over age 50, but it’s not clear why some women get breast cancer (including women with no risk factors) and others do not (including those who do have risk factors).
Some breast cancer risks may be preventable. Of course, you cannot control every variable that may influence your risk. Here are the key breast cancer risk factors to know.
- Age and gender. If you are a woman and you’re getting older, you may be at risk of developing breast cancer. The risk begins to climb after age 40 and is highest for women in their 70s.
- Family history. Having a close blood relative with breast cancer increases your risk of developing the disease. A woman’s breast cancer risk is almost double if she has a mom, sister, or daughter with breast cancer and about triple if she has two or more first-degree relatives with breast cancer.
- A breast cancer gene mutation. Up to 10% of all breast cancers are thought to be inherited, and many of these cases are due to defects in one or more genes, especially the BRCA1 or BRCA2 genes. (Scientists are studying several other gene mutations as well.) In the U.S., BRCA1 and BRCA2 mutations are more common in Jewish women of Eastern European descent. Having these defective genes doesn’t mean you will get breast cancer, but the risk is greater: A woman’s lifetime risk of breast cancer with a BRCA1 gene mutation, for example, may be more like 55% to 65% compared to the average 12%.
- Breast changes and conditions. Women with dense breasts or with a personal history of breast lumps, a previous breast cancer, or certain non-cancerous breast conditions are at greater risk of developing breast cancer than women who do not have these conditions.
- Race/ethnicity. White women are slightly more likely to develop breast cancer than Asian, Hispanic, and African American women. But African American women are more likely to develop more aggressive breast cancer at a younger age and both African American and Hispanic women are more likely to die from breast cancer than white women.
- Hormones. Women with early menstrual periods (starting before age 12) and late menopause (after age 55) are at greater risk of getting breast cancer. Scientists think their longer exposure to the female hormone estrogen may be a factor, because estrogen stimulates growth of the cells of the breast. Likewise, use of hormone therapy after menopause appears to boost the risk of breast cancer. Oral birth control pills have been linked to a small increase in breast cancer risk compared with women who never used hormonal contraception. But that risk is temporary: More than 10 years after stopping the pill, a woman’s breast cancer risk returns to average.
- Weight. Women who are overweight or obese after menopause are more likely to get breast cancer. The exact reason why isn’t clear, but it may be due to higher levels of estrogen produced by fat cells after menopause. Being overweight also boosts blood levels of insulin, which may affect breast cancer risk.
- Alcohol consumption. Studies suggest women who drink two or more alcoholic beverages a day are 1 1/2 times more likely than non-drinkers to develop breast cancer. The risk rises with greater alcohol intake, and alcohol is known to increase the risk of other cancers too. For that reason, the American Cancer Society (ACS) recommends that women stick to one drink a day–or less.
- Radiation exposure. A woman’s risk of developing breast cancer may be higher than normal if she had chest radiation for another disease as a child or young adult.
- Pregnancy history. Having no children or having a first child after age 30 may increase your risk of breast cancer.
- DES exposure. Women who were given the now-banned drug diethylstilbestrol to prevent miscarriage decades ago face a slightly increased risk of breast cancer, as do their daughters.
Scientists are studying a slew of other factors to determine what role, if any, they may play in the development of breast cancer. There’s not enough evidence to say for sure whether smoking, dietary fat, or environmental exposure to certain chemicals, for example, ramp up the risk for breast cancer because study results to date are mixed.
Breast cancer symptoms
Breast cancer symptoms vary from one person to the next. Knowing what your breasts normally look and feel like may help you recognize possible signs and symptoms.
What does breast cancer feel like? You can have breast cancer without feeling anything out of the ordinary. But, if you find an area of thickening breast tissue, a lump in your breast (usually painless, but not always) or an enlarged underarm lymph node, see your physician.
RELATED: The 15 Worst Things You Can Say to Someone With Breast Cancer
What does breast cancer look like? You may notice a change in the shape or size of your breast. You could have an area of skin that dimples or a nipple that leaks fluid.
Often, there are no early warning signs of breast cancer. Even if you develop a lump, it may be too small to feel. That’s why breast cancer screening, typically using mammography, is so important. Early signs and symptoms of breast cancer that some women and men might experience include:
- New lump in the breast or armpit, with or without pain. Lumps are often hard but can be soft as well. (Not all lumps are breast cancer. Some lumps may be noncancerous changes or benign, fluid-filled cysts, but they should be checked by your physician.)
- Change in breast size or shape. Look for swelling, thickening, or shrinkage, especially in one breast.
- Dimpling, pitting, or redness. Breast skin may take on the appearance of an orange peel.
- Peeling, flaking, or scaling breast skin.
- Red, thick, or scaly nipple.
- Breast, nipple, or armpit pain.
- Inverted nipple. Look for a nipple that turns inward or flattens.
- Nipple discharge. It may be clear or bloody.
- Redness or unusual warmth. This can be a sign of inflammatory breast cancer, a rare and aggressive form of the disease.
- Swollen lymph nodes under the arm or around the collarbone, which could be a sign that breast cancer has spread.
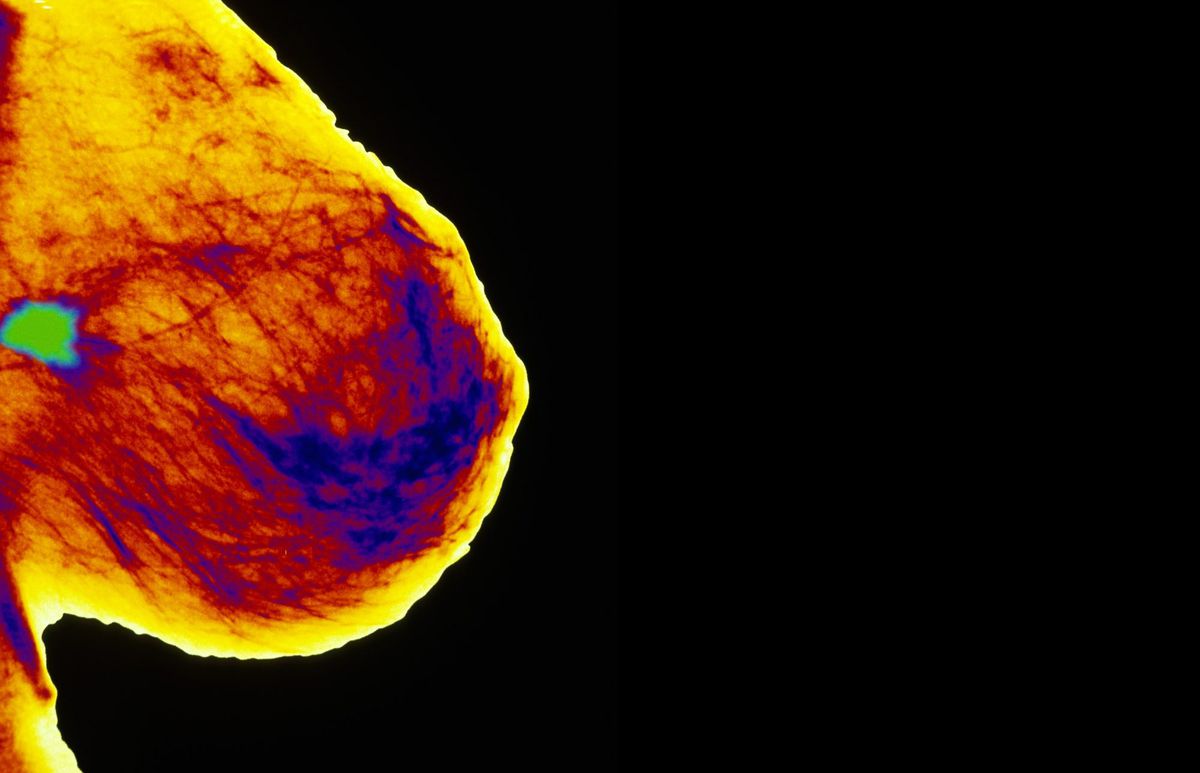
 GettyImages-157672425 or how frequently women should be tested.
GettyImages-157672425 or how frequently women should be tested.
The National Comprehensive Cancer Network (an alliance of cancer centers) recommends annual screening beginning at age 40.
The ACS says women ages 40 to 44 should have the option to begin screening every year. It recommends annual screening for women ages 45 to 54. At 55, a woman can decide to continue annual screening or go for her mammogram every other year for as long as she is healthy and has 10 more years of life to live.
The U.S. Preventive Services Task Force advises women 40 to 49 to talk to their health care provider about when to start screening and how often to be screened. For women 50 to 74, it recommends a mammogram every two years.
Women at high risk of developing breast cancer should be screened earlier and more often. The ACS recommends annual mammograms and breast MRIs starting at age 30 for women with a higher-than-average risk of developing breast cancer, including those with a known breast cancer gene mutation or a first-degree relative with an inherited breast cancer gene mutation.
RELATED: 25 Breast Cancer Myths Busted
Since men have less breast tissue and less breast cancer, they are not routinely screened for the disease. If there is a strong family history of breast cancer or a known breast cancer gene mutation in the family, a man might consider having genetic testing to see if he has a mutation that increases his risk for male breast cancer.
Men who are at high risk for breast cancer should talk to their health care provider about having their breasts examined during routine checkups and doing breast self-exams.
Male or female, it is helpful to know what your breasts normally look and feel like so that you can report any changes to your doctor. The American College of Obstetricians and Gynecologists recommends “breast self-awareness,” meaning knowing what’s normal for your own breasts and paying attention to any changes you may feel.
Regular breast self-exams are no longer recommended as a routine screening method for women because there isn’t sufficient evidence that they offer any early detection or survival benefits.
But should women still have their breasts examined by a doctor every year? Some medical groups see no clear benefit of a clinical breast exam, while others continue to recommend one every year as part of a routine checkup.
Diagnosing breast cancer
An abnormal finding on a screening mammogram or discovering a lump or other breast changes doesn’t necessarily mean you have breast cancer.
First, your doctor will need to perform follow-up testing using one or more types of scans. A diagnostic mammogram, which involves more X-rays than a screening mammogram, can offer a more detailed view of the area of concern. Two other tests, a breast MRI or a breast ultrasound, may be ordered to gather additional diagnostic information.
There is only one way to confirm a cancer diagnosis. You will need a biopsy to extract cells or tissue from the area of the breast that is causing concern. A fine needle may be used to remove cells or tissue, or you may undergo a surgical procedure to remove a piece of breast tissue.
A pathologist will use these specimens to look for cancer under a microscope and may perform additional testing on the tissue sample. The pathology findings can confirm whether or not you have breast cancer and what your chances of beating it–your prognosis–may be. This information can help your medical team (your doctor, your surgeon, your radiologist, and other providers) determine the best course of treatment.
 types-of-cancer Cancers that are positive for estrogen receptors, progesterone receptors, and HER2 can be treated with hormone therapies and drugs that target HER2.
types-of-cancer Cancers that are positive for estrogen receptors, progesterone receptors, and HER2 can be treated with hormone therapies and drugs that target HER2.
Breast cancer stages
All breast cancers are assigned a stage based on biopsy results plus other findings from blood tests and imaging scans. Staging can help you and your medical team make decisions about appropriate treatment and understand your chances of survival.
RELATED: 22 Ways to Help a Friend With Breast Cancer
Breast cancer stages reflect the size of the tumor, whether it is invasive, whether it has reached the lymph nodes (glands that are part of the body’s immune system), and whether it has spread to other parts of the body.
Stage 4 breast cancer
At Stage 4, breast cancer has traveled to distant sites in the body, often the bones, liver, brain, or lungs. This is called metastatic breast cancer. Although this stage is considered incurable, new treatments allow patients to live longer with their disease.
Stage 3 breast cancer
Stage 3 breast cancer is an advanced cancer. It’s in the lymph nodes but has not spread to other organs. This stage is divided into three categories, 3A, 3B and 3C, based on the size of the tumor and how many and which lymph nodes are involved.
Stage 2 breast cancer
At Stage 2, breast cancer is growing but is only in the breast or nearby lymph nodes. This stage has two categories, 2A and 2B, based on how large the tumor is and whether or not it has spread to nearby lymph nodes.
Stage 1 breast cancer
Stage 1 is an invasive cancer, meaning it is invading healthy breast tissue, but it has not spread outside the breast. This stage also has two categories, 1A and 1B, based on whether there is any evidence of small clusters of breast cancer cells in nearby lymph nodes.
Stage 0 breast cancer
Also called pre-cancer, this is the earliest stage of breast cancer. It involves abnormal cells that have not spread into breast tissue from the ducts or lobules where they began. Stage 0 breast cancer also has not spread to lymph nodes or other parts of the body. Stage 0 breast cancer is non-invasive, like ductal carcinoma in situ (DCIS).
 GettyImages-530685029
GettyImages-530685029
Radiation therapy uses high-energy waves to kill cancer cells and shrink tumors. It may be recommended for patients who have breast cancer surgery or whose cancer has spread to other parts of the body.
Cancer-killing chemotherapy medicines are delivered intravenously (into a vein) or taken by mouth. Chemo may be given before or after surgery. It’s also used in treating advanced cancer cases. Because these medicines travel through the bloodstream, they can have significant side effects, including mouth sores, hair loss, nausea, vomiting, and diarrhea.
Some breast cancers are sensitive to hormones produced in the body. In these hormone receptor-positive breast cancers, estrogen and/or progesterone fuels cancer growth. Hormone therapy can lower the body’s estrogen levels or stop hormones from binding to cancer cells. This category of breast cancer treatment includes the oral medicine tamoxifen, which is often given after surgery to women with hormone receptor-positive breast cancer.
Newer medicines, called targeted therapies, specifically attack cancer cells while sparing normal cells, meaning patients experience fewer side effects. Trastuzumab (Herceptin), for example, is a drug that starves HER2-positive breast cancers by blocking the HER2 protein.
Treatment outcomes may depend on the stage of cancer, a patient’s response to treatment, and other factors.
Generally speaking, stage 0 and 1 breast cancers are highly treatable. The five-year survival rate for women diagnosed with breast cancer in these early stages is close to 100%. At stages 2 and 3, some 93% and 72% of women, respectively, can expect to live at least five years after being diagnosed with breast cancer. Stage 4 or metastatic breast cancer is difficult to treat. The five-year survival rate is about 22%.
For men with breast cancer, the five-year survival rates are similar: 100% for stages 0 and 1, 91% for stage 2, 72% for stage 3, and 20% for stage 4.
Remember, breast cancer statistics are just averages. They don’t reflect an individual patient’s experience.
Breast cancer prevention
While no one can tell you how to prevent breast cancer with any sort of guarantee, there’s evidence to suggest that certain healthy lifestyle changes can lower your breast cancer risk.
- Limit your alcohol intake. The more you drink, the higher your risk of breast cancer.
- Watch your weight. Being overweight or obese boosts your breast cancer risk.
- Exercise. Women who work out regularly have a lower risk of breast cancer than less active women.
- Consider breastfeeding your baby. Women who breastfeed have a lower risk of breast cancer than moms who do not breastfeed their children.
- Reduce your hormone intake. Hormone therapy users are at higher risk for breast cancer. If you’re taking hormones to relieve menopausal symptoms, talk to your doctor about taking the lowest dose that works for you for the shortest time.
RELATED: Celebrities Who Battled Breast Cancer
Patient advocates hope that greater breast cancer awareness will lead to earlier detection and better outcomes. You, too, can join the fight against breast cancer. October is National Breast Cancer Awareness Month, a great time to join a breast cancer walk near you.
