:max_bytes(150000):strip_icc()/Chlorine-7caa4779df9d46d09bf8b6a05f243bca.jpg)
:max_bytes(150000):strip_icc()/Chlorine-7caa4779df9d46d09bf8b6a05f243bca.jpg)
Oleg Breslavtsev / Getty Images
Chlorine is a chemical disinfectant added to swimming pools to kill germs. In its original gas form, chlorine is a highly irritating and damaging chemical. When added to pool water, chlorine technically turns into the chemicals hypochlorous acid and hypochlorite anion, which disinfect water and is considered safe in the right concentration.
That said, frequent swimmers may find that chlorinated water causes unwanted side effects. When chlorine concentration is too high, it can also cause allergy-like symptoms. Here are five ways chlorine can affect your body.
How Much Chlorine Is Safe?
Adding a chlorine concentration of at least 1 part per million (ppm) to pool water—and 3 ppm in hot tubs—is considered safe by the Centers for Disease Control and Prevention (CDC).
In the U.S., most local health departments require pools to have a combined chlorine level of 0.4 ppm or less. Combined chlorine is chlorine that has already bound itself with germs and waste to disinfect the pool.
It May Cause Dry Skin and Rash
Chlorine and other chemicals in pool water can irritate and dry out the skin. People can’t be allergic to chlorine, but you can be sensitive to the chemical and have skin reactions that are actually irritant dermatitis caused by hypersensitivity to chlorine.
Chlorinated water can cause irritating skin symptoms like:
- Dry, itchy skin
- Red skin
- Hives or rash
- Eczema or psoriasis flare-ups
- Dry skin that triggers acne
Research shows that frequent swimmers are more prone to allergic contact dermatitis or “pool water dermatitis.” This itchy rash is caused by pool chemicals like chlorine. However, some people may get rashes from swim gear like swim caps and goggles rubbing on the skin.
If you have psoriasis, an autoimmune skin disorder that causes thick patches of discolored skin and silver scales, dipping in the pool can further aggravate your psoriasis plaques. Chlorine can also worsen symptoms of eczema, a skin disorder that causes dry and itchy patches of skin.
If your skin is sensitive to chlorine, the American Academy of Dermatology suggests:
- Moisturizing your skin before jumping in the pool
- Rinsing off with warm water after you finish swimming
- Gently patting with a towel to dry off
- Apply moisturizer to damp skin
A Chlorine Rash Might Make Your Skin Feel Itchy After Swimming in a Pool
It May Lead To Lightened and Dry Hair
Chlorinated water dissolves oils that coat and protect your hair, which may make your hair more prone to damage and dryness. Chlorine also breaks down proteins in your hair, increasing your risk of hair breakage. People with white or blonde hair are more at risk because the hair has less melanin (what gives skin and hair color) to protect it.
Chlorine can also lighten your hair, especially if the pool water you swim in has a high concentration of chlorine. (For context, bleach, known to lighten hair and laundry stains, is made with chlorine.) Lightening hair requires high chlorine concentrations, so it takes time and lots of swimming to see the effects. However, UV light from the sun can also lighten hair and increase the impact of chlorine on hair.
To keep your hair healthy while you swim, the AAD suggests you:
- Apply oil or leave-in conditioner to your hair before you swim
- Wear a swim cap to keep hair away from chlorine
- Rinse your hair before swimming to help avoid chlorine absorption
- Rinse and wash your hair after swimming with a shampoo designed to remove chlorine and following up with a deep conditioner
Chlorine Doesn’t Turn Your Hair Green
Oxidized copper is what turns blonde or white hair green after a swim. Copper sulfate is sometimes added to pools to control algae growth. Copper can also leak into the pool from plumbing or copper ionizer equipment. Chlorine corrodes copper that sticks to the hair, resulting in a similar green-blue color of copper patina.
It May Cause Respiratory Issues
High levels of combined chlorine release chloramines into the water and air, which can be highly irritating. Combined chlorine is chlorine that has bound to germs and waste to disinfect the pool.
Chlorinated pools don't usually cause respiratory problems. However, if a pool has built up high levels of chloramines, you can experience respiratory issues like:
- Coughing
- Wheezing
- Asthma attack
- Itchy, runny, or stuffy nose
Pools build up chloramines when chlorine mixes with sweat, dirt, poop, pee, and dead skin cells. Even jumping in the pool with deodorant or makeup can create chloramines.
Chloramines also turns into gas around the pool area. A pool that has built up too many chloramines often has a strong chemical smell, which people mistakenly call a "chlorine smell." The chloramines in the air are usually responsible for respiratory issues during or after swimming. This is more common in indoor pools because they are not as well-ventilated to allow chloramine to leave the area.
How Long After Shocking a Pool Is It Safe To Swim?
It May Cause Eye Irritation
Chlorine and other pool chemicals can wash away the thin layer of tears that coat your eyes. As a result, chlorine can cause eye side effects like:
- Burning
- Itching
- Redness
- Watery feeling
- Dry eyes
- Gritty feeling
- Blurry vision
Chloramines released when chlorine combines with human waste also irritate the eyes. Swimmers in a pool with built-up chloramines may experience eye irritation like red, itchy eyes.
The American Academy of Ophthalmology suggests rinsing your eyes with fresh water after swimming to help remove chlorinated water from your eyes. Eye drops may also help rebalance any tears, and wearing goggles keeps chlorinated water out of your eyes.
It May Lead to Yellow Teeth
Chlorine and other pool chemicals can cause people’s teeth to form yellow and brown stains, known as swimmer’s calculus. This staining happens because the pH of chlorinated pools is higher than your saliva, which breaks down proteins that protect teeth from straining and tartar build-up. Chlorinated pools can also erode enamel, which makes you more likely to deal with staining.
However, it's unlikely your teeth will turn yellow after visiting your local pool a few times a week. Research shows competitive swimmers and divers—especially those who spend more than six hours a week in the pool—are more likely to develop yellow teeth.
U.S. Masters Swimming recommends brushing your teeth before swimming to help prevent pool chemicals from building up on plaque. After a swim, rinse your mouth with fresh water or fluoride mouthwash to help restore your mouth's pH levels. Brushing may be too harsh on your enamel after a swim.
A Quick Review
Chlorinated water is considered safe when pools have the correct concentration of chlorine. However, some people are more sensitive to chlorine. Chlorine can irritate the eyes, skin, hair, and teeth.
Occasionally swimming doesn't cause significant side effects, but people who swim frequently are more likely to experience chlorine side effects.
Pools with too high chlorine levels and built-up chloramines can also irritate the respiratory system. If you have issues breathing or have intense allergy-like symptoms, ask the pool manager to check the chlorine levels.
]]>People with psoriasis usually begin to notice their plaques develop on the knees, elbows, and scalp. Sometimes, plaques can spread to the hands, feet, and areas of the body where your skin folds (e.g., under your arms and breasts). Symptoms can develop at any age, but most people with psoriasis start developing plaques between the ages of 15 and 35.
Scientists do not yet know what causes psoriasis, as research is still underway. However, researchers do know that the condition is not contagious and that your immune system functioning and genetics play a large role in whether you will develop the condition. In some cases, environmental factors can also trigger the onset of symptoms or lead to psoriatic flare-ups.
:max_bytes(150000):strip_icc()/Health-GettyImages-1486105992-6fef9bd4792647039e3bbf22e282f4ea.jpg)
:max_bytes(150000):strip_icc()/Health-GettyImages-1486105992-6fef9bd4792647039e3bbf22e282f4ea.jpg)
Jose Araujo / Getty Images
Immune System Functioning
Since psoriasis is an autoimmune condition, researchers believe that an overactive immune system speeds up skin cell growth. When the immune system is functioning properly, skin cells typically take about a month to grow completely and then shed. With psoriasis, skin cells can grow within three to five days. After the cells are done growing, instead of shedding, they pile up on the skin and develop into dry plaques.
Research suggests that the overgrowth of skin cells occurs because of an issue with your T-cells, or white blood cells. T-cells are an important part of the immune system. They help keep you safe by fighting bacteria, viruses, and other harmful things that enter the body.
However, if you have psoriasis, your T-cells attack healthy skin cells by mistake. As a result, your body reacts by making new skin cells more frequently, which eventually turn into plaques and scales on the skin.
How Nail Pitting Can Be a Sign of Psoriasis
Genetics
While people can develop psoriasis without having a family history of the disease, a 2020 study found that a family history of psoriasis and psoriatic arthritis can make you more likely to develop the condition.
Research also suggests that if you have one parent that has psoriasis, you have a 28% chance of also developing symptoms. Your likelihood of developing the condition rises to 65% when both parents have psoriasis.
What Is Psoriatic Arthritis?
Psoriatic arthritis is an autoimmune disease that typically develops in people who have psoriasis. People with psoriatic arthritis experience joint symptoms such as pain, inflammation, and stiffness.
Research about the connection between psoriasis and genetics is still ongoing. Even if you have a gene linked to psoriasis, it doesn’t always mean you will get the condition. Alternatively, there are people with psoriasis who don’t have genes associated with psoriasis but still develop symptoms. This is why experts think environmental factors can also contribute to the onset of psoriasis symptoms.
How To Prevent Psoriatic Arthritis
Environmental Triggers
In some cases, you may experience psoriasis symptoms or flare-ups due to a variety of environmental triggers. These factors can vary from person to person and not all triggers affect everyone the same way.
- Stress: Stressful life events (e.g., job loss or divorce) and daily stressors (e.g., being stuck in traffic or studying for a big test) can cause a psoriasis flare-up. However, eliminating all stress from your life isn’t a realistic goal. Instead, using stress management techniques like meditation, exercise, or journaling, can help you manage stress better and reduce flare-ups.
- Injury: Cuts, scratches, and severe sunburns are all types of skin injuries that can lead to the onset of symptoms. Research shows that skin injuries can cause new plaques and lesions on the skin. This is a result of the Koebner phenomenon which suggests that injury to the skin can lead to a psoriatic flare-up.
- Illness: Due to the autoimmune nature of psoriasis, any illness that triggers the immune system can cause symptoms. Illnesses such as strep throat, bronchitis, and ear infections may trigger a flare-up. Generally, children may be more susceptible to illness-related flare-ups. However, an illness can lead to the onset of symptoms in adults, too.
- Cold and dry weather: Research suggests that the lack of sunlight and humidity that is associated with colder weather can trigger psoriasis flare-ups. For some people, cold weather can lead to dry or flaky skin and worsen symptoms. If weather affects your symptoms, warmer and more humid weather can improve symptoms and reduce flares.
- Lifestyle behaviors: Drinking alcohol, using tobacco, taking certain medications, shaving, and getting tattoos can sometimes lead to flare-ups. Each of these lifestyle factors varies from person to person. It can take some time to learn what triggers your flare-ups and that’s OK. To help you better understand what your triggers are, keeping a log of your symptoms and what may have triggered them can help.
Key Differences Between Eczema and Psoriasis You Need to Know
A Quick Review
Like other autoimmune diseases, researchers are still investigating the exact cause of psoriasis. Here’s what they do know: a combination of an overactive immune system, a genetic link to psoriasis, having a family history, and exposure to environmental triggers like stress or illness may all contribute to the onset of symptoms.
If you suspect that you may have psoriasis symptoms, it’s a good idea to visit your healthcare provider for an examination and a proper diagnosis.
]]>A spike in opioid-related deaths in the US, per new government data, highlights the need for expanded access to therapies. Here's what to know if you're seeking medication-assisted treatment or therapy for opioid addiction or dependence.
What is an opioid use disorder?
The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders defines opioid use disorder as "a problematic pattern of opioid use leading to problems or distress." You might be diagnosed with this condition if you experience two or more of the following symptoms over a 12-month period:
- Taking opioids at a higher quantity or longer than prescribed
- Regularly working to limit or stop opioid use without success
- Spending large amounts of time taking opioids or working to procure them
- Continuing to take opioids even when they bring social or interpersonal problems
- Struggling to fulfill life obligations
- Foregoing or limiting participation in certain activities due to opioid use
- Taking opioids in a physically hazardous situation
- Craving or strong want for opioids
- Taking opioids, even if they cause or increase physical or psychological problems
- Increasing tolerance throughout the use of opioids
- Feeling withdrawal after stopping use of opioids
"Opiates provide an innate calming effect on both the body and brain system. When they are prescribed for pain, they specifically target those areas. However, if misused, this is where we oftentimes see problems arise," Chris Gleason, the executive director at Brightside Recovery in Tinley Park, Illinois, tells Health.
RELATED: Opioid Drugs: A List of Common Prescription and Street Drugs, According to Experts
How is opioid use disorder treated?
Opioid use disorder, like diabetes, is a chronic disease that requires ongoing, varied forms of treatment, explains Jeanmarie Perrone, MD, a professor of emergency medicine and director of the division of medical toxicology and addiction medicine initiatives for the Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
"Patients who are on diabetes medicine could still come in with high blood sugar. And we don't say, well, that's your fourth time here with high blood sugar; we're not going to treat you at all anymore," Dr. Perrone tells Health.
There are multiple treatment options available once a person is ready to seek help for an opioid use disorder. Medical professionals may provide these treatments during in- or residential stays or through outpatient care.
Medication-assisted treatment
Medications for opioid use disorder can decrease opioid use, lower relapse rates, increase the rate of treatment retention, and lower rates of opioid-related overdose deaths, among other benefits, says " Elizabeth Evans, MD, a psychiatrist and addiction specialist at Columbia Doctors Midtown in New York City, tells Health.
There are three medications approved by the US Food and Drug Administration for opioid use disorder treatment:
Methadone
Methadone is an opioid agonist that reduces cravings and withdrawal symptoms by activating opioid receptors. It also limits, or even stops opioids' effects, reports John Hopkins Medicine. It is only available through a Substance Abuse and Mental Health Services Administration (SAMHSA)-certified treatment program. Administrators will provide the medication daily, but if a person demonstrates compliance and progress, they may be able to take doses at home.
Buprenorphine
Buprenorphine works similarly to methadone but is a partial opioid agonist meaning it still "binds to opioid receptors but activates them less strongly than full agonists do," says Dr. Evans. Unlike methadone, buprenorphine is available by prescription.
A 2018 study from Annals of Internal Medicine looked at how taking methadone or buprenorphine impacted overdose risk in people who had overdosed between 2012 and 2014. Across a 12-month follow-up period, deaths due to an opioid overdose decreased in people taking methadone by 59% and buprenorphine by 38%, compared to participants without medication-assisted treatment.
Naltrexone
This drug is somewhat different than its counterparts. It does not activate opioid receptors. Instead, it prevents opioids "from producing rewarding effects such as euphoria, and it can also help with cravings," says Dr. Evans.
The other big difference: a person can only take naltrexone if their system is free of opioids. Per the US National Library of Medicine (NLM), your doctor will tell you not to start naltrexone if you've used opioids in the past seven to 10 days. It is available in a prescription pill or an administered monthly long-acting injection.
RELATED: 8 Opioid Overdose Symptoms and What to Do If You Suspect That Someone Has ODed
Emergency Medication
Naloxone is not a treatment but an emergency preventative measure.
"Naloxone can quickly restore normal breathing to a person if their breathing has slowed or stopped because of an opioid overdose. Naloxone has no effect on someone who does not have opioids in their system," says Dr. Evans.
Carrying naloxone is important for anyone with an opioid use disorder, a loved one who does, or if you want to be prepared in general. Individuals can obtain free naloxone kits at many pharmacies, community-based distribution programs, local public health groups, or local health departments. Many of these organizations and those online offer training courses.
RELATED:14 Symptoms of Opioid Withdrawal—and What to Know About Breaking Your Addiction
Therapies for opioid use disorder
There are two forms of therapy anyone with an opioid use disorder may wish to pursue: individual and group.
According to the NLM, people may try cognitive-behavioral therapy, motivational enhancement therapy, or contingency management in a one-on-one setting with a mental health professional.
"Structured behavioral therapies focus on helping motivate individuals towards change, helping them to develop skills to manage triggers and cravings, as well as identify ways to develop and engage in a life that is meaningful to them," says Dr. Evans.
People can also attend group therapy to learn and gain support from others dealing with an opioid use disorder. Family counseling can help repair relationships and show loved ones how to best support you.
RELATED: 14 Symptoms of Opioid Withdrawal—and What to Know About Breaking Your Addiction
Seeking treatment for opioid use disorder
Although anyone could develop an opioid use disorder, the stigma associated with it may deter some people from getting medical help.
"We need to continue to treat this as a disease," says Dr. Evans. "By taking a disease management approach, we can help others to understand that this is simply not a moral failing or a behavior problem that has roots in medical disease."
Various environmental motivators may lead a person to seek treatment. According to Dr. Perrone, these factors include facing a breaking point with a family member or a loved one or partner, becoming tired of missing out on valuable things, and incurring the expense of opioids, which can cause loss in other areas of their life.
"Most people should seek treatment at the onset of any type of withdrawal so that they can be medically managed and decrease the severity," says Gleason.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>"Wearing your disease on the outside of your body can be very difficult, which is why it's wonderful that we have so many treatments that we can use to make people better," Robert T. Brodell, MD, chair of the department of dermatology at the University of Mississippi Medical Center, tells Health.
From topical treatments and light therapy to medications that work within the body, rest assured that there are plenty of ways to take control of your psoriasis.
"Over the past 20 years, we've seen a lot of advancements in treatments. Your dermatologist has many options to tailor treatment for you," says Dr. Brodell.
RELATED: What Does Plaque Psoriasis Look Like? Here's What to Look For, According to Experts
How do dermatologists treat plaque psoriasis?
Although there is no cure for psoriasis, Adam Friedman, MD, professor of dermatology at George Washington School of Medicine and Health Sciences, says there is almost always a treatment option that can help.
If, after seeking treatment, you're still experiencing symptoms and flare-ups of your moderate-to-severe psoriasis, but your doctor isn't offering you another option, that should be a warning sign to you, says Dr. Friedman. "We know under-treatment is a problem," he tells Health.
Here are three categories of treatment that dermatologists commonly recommend, plus several non-traditional remedies that experts say may be worth a try. Your doctor may use one, or a combination of the following, to bring you relief.
Topical treatments
Topical treatments, such as steroid creams to reduce swelling and redness, are often what many doctors try first when treating plaque psoriasis, no matter which part of the body it presents on.
"A strong topical treatment is what we might start with if someone has localized psoriasis, and if no progress is made, we'll move on," says Dr. Brodell.
Some topicals are available by prescription only, while others can be purchased over-the-counter, says the National Psoriasis Foundation (NPF).
In addition to steroids, this treatment category includes non-steroidal options (such as calcipotriene, a synthetic form of vitamin D for scalp and nail psoriasis) and over-the-counter lotions, creams, shampoos, and bath products.
The NPF says some OTC treatments contain these active ingredients approved by the US Food and Drug Administration for psoriasis treatment:
- Salicylic acid, which works by softening plaques and scales and removing them from the skin.
- Tar (made from coal or wood), which slows skin cell growth and reduces inflammation, itching, and scaling.
A word of caution, though: Tar can irritate the skin. And some people (including those who are pregnant or breastfeeding) should avoid using it, says the American Academy of Dermatology Association (AAD).
To ensure that OTC products are not irritating and are safe to use for psoriasis, review NPF's Seal of Recognition program.
RELATED: What Is Inverse Psoriasis—and What's the Best Way to Treat It?
Light therapy
By shining ultraviolet (UV) rays on the skin, light therapy (aka phototherapy) can help skin cells grow more slowly. The AAD explains that this form of treatment can help with psoriasis because it suppresses the immune system, which in turn can reduce inflammation, allowing the skin to heal and stop itching.
While Dr. Friedman says light therapy can be an effective treatment for the skin, he points to a key limitation: "It works pretty well for skin disease, but doesn't have an effect on joint disease or underlying medical problems associated with psoriasis."
Additionally, having to go to an office a few times a week to receive the therapy can deter people, he says. The question is whether that's even necessary. A large randomized controlled trial, called the LITE Study, funded by the independent, nonprofit Patient-Centered Outcomes Research Institute, will compare the safety and effectiveness of 12 weeks of at-home versus office-based UVB phototherapy for the treatment of psoriasis. "We're trying to see if getting the treatment at home is a viable option," says Dr. Friedman, whose institution is among the trial sites.
UV light treatments aren't without side effects. As AAD notes, your skin may be red and tender (like a sunburn) afterward, and people with medium-to-dark skin may develop dark spots.
RELATED: Psoriasis Causes, Plus 7 Things That Can Cause Symptom Flare-Ups, According to Dermatologists
Systemic medications
If you've tried topical treatments or light therapy with no relief, your doctor may move on to prescribing oral medicines or biologics, says the NPF.
Either by prescription or over-the-counter, oral medicines work within the body to slow down the immune system. Options include methotrexate, synthetic vitamin A, apremilast (Otezla), tofacitinib (Xeljanz), and others, says the NPF.
Doctors may also try one of a slew of intravenous and injectable biologics that target specific areas of the body. The NPF says these include certolizumab pegol (Cimzia), ixekizumab (Taltz), guselkumab (Tremfya)—and the list goes on.
"There are now 13 or 14 biologic drugs, which are targeted therapies that keep most of your immunity functioning normally," says Dr. Brodell. "Targeted therapies for some patients are almost magical in the way they can knock down psoriasis."
Oftentimes doctors will rotate among several systemic drugs to find the one that works best for you, he says.
As with any medications you take, it's important to discuss the potential side effects with your doctor.
Do complementary and alternative approaches work for plaque psoriasis?
Plenty of people with psoriasis turn to non-traditional therapies for relief. Responding to a 2019 patient survey described in the Journal of the American Academy of Dermatology, 41% of patients reported using alternative treatments in place of traditional medicine in the last five years, while 50% said that they have added complementary remedies to their treatment regimen.
When used in combination with traditional treatments, some people find that integrating natural treatment can be helpful, says the NPF. But some remedies can interact with medications or might not be a good fit for you, so it's important to talk with your doctor first. Below are some options.
Aloe vera. This plant gel may help reduce redness and scaling caused by psoriasis and can be applied up to three times a day, according to the NPF. The foundation suggests finding a cream containing 0.5% aloe.
Apple cider vinegar. Applying apple cider vinegar a few times a week can help with itching on the scalp that is caused by psoriasis, as long as you don't have cracked skin or bleeding areas on the scalp. To avoid burning, the NPF recommends using organic apple cider vinegar that is diluted with water in a one-to-one ratio.
Capsaicin. When added to creams and ointments, this ingredient derived from chili peppers can block nerve endings that cause pain, says the NPF. Other benefits? It may quell inflammation and reduce redness and scaling, it says. However, the foundation cautions that more research is needed on capsaicin's long-term benefits and safety.
Sea salt. Adding Dead Sea or Epson salt to a warm, 15-minute bath can help scales fall off and relieve itching, says the NPF.
Turmeric. The NPF cites research suggesting that curcumin, the active ingredient in turmeric, has antioxidant and anti-inflammatory properties that may benefit some people by reducing their psoriasis and psoriatic arthritis flare-ups. Turmeric and curcumin products taken orally or applied topically in recommended amounts "are probably safe," says the National Center for Complementary and Integrative Health (NCCIH). However, these products may be unsafe when used by pregnant people in amounts greater than what's found in food, and little is known about its safety during breastfeeding, says NCCIH.
RELATED: Is There a Diet for Psoriasis? 5 Foods That May Be Beneficial, and 5 That Probably Aren't
Mahonia. This antimicrobial herb can help mild-to-moderate psoriasis when applied to the skin, says the NPF, which suggests using a cream with 10% mahonia. A 2018 review in the Journal of Clinical and Aesthetic Dermatology identified several studies in which mahonia use was associated with significant symptom improvement and minimal side effects.
Physical therapy and massage. Physical therapy can be used to help with psoriatic arthritis by increasing mobility in joints. Because massage can help loosen and stretch muscles and joints, the NPF says it can be helpful for those with psoriasis and psoriatic arthritis.
Acupuncture. Acupuncture involves inserting needles into certain spots on the body with the intention of relieving symptoms in those areas. A 2018 systematic review in JAMA Dermatology noted that this traditional Chinese therapy appears to be beneficial for the treatment of psoriasis. But based on existing studies, it's difficult to determine the most effective technique for treating psoriasis, according to the review.
Mind-body therapies. Since stress can trigger psoriasis flare-ups, researchers have examined the role of meditation and relaxation techniques using guided imagery, for example. Based on a small number of studies, it appears that these mind-body interventions may be a beneficial, complementary treatment, per the JAMA Dermatology review.
Indigo naturalis. Applied topically, this derivative of indigo plants has been shown to be safe and effective for treating psoriasis, says the AAD. The JAMA Dermatology review says there's reasonable evidence to recommend trying this traditional Chinese medicine (also known as qing dai), but says the optimal dosage is uncertain and cautions consumers that it may be difficult to find a reputable source of this product.
Cannabis. Dr. Friedman says the effects of medical cannabis for those with psoriasis is being studied. "There is pre-clinical data about how it could be anti-inflammatory, but we don't have a lot of information," he says.
To get more inspiring stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>Of course, whether surgery is appropriate may depend on the area of your body that's affected. A surgeon can readily access sweat glands in your armpit because they are near each other, says Dee Anna Glaser, MD, dermatologist at SLUCare Physician Group. By contrast, the skin on your feet and on the palms of hands is tough and difficult to penetrate.
Keep in mind that surgery is not a panacea. Sweat glands are tiny and sometimes hard to detect with instruments, Dr. Glaser tells Health, so it can be hard to predict the success of a surgical procedure.
So is surgery an option for you? Here's what to know about surgical treatments for hyperhidrosis.
 hyperhidroisis surgery —sweating in the armpits—requires local anesthesia and can be done in an office setting rather than a hospital. You doctor might recommend one or a combination of the following, says Dr. Glaser:
hyperhidroisis surgery —sweating in the armpits—requires local anesthesia and can be done in an office setting rather than a hospital. You doctor might recommend one or a combination of the following, says Dr. Glaser:
- Excision, which involves the surgeon cutting out sweat glands from your underarms.
- Curettage, which involves the surgeon scraping out sweat glands in your armpit area.
- Liposuction, which involves suctioning out sweat glands in the underarms.
"In each of these surgeries, the surgeon is trying to remove or injure the sweat glands, so they don't produce sweat anymore," Adam Friedman, MD, professor of dermatology at George Washington School of Medicine and Health Sciences, tells Health.
While the International Hyperhidrosis Society (IHS) states that these surgeries often have good results, it warns that they are permanent and, therefore, not reversible.
Recovery time typically takes a few days, with some soreness that can last up to a week. You may need to hold off on using your arms to lift things or engage in physical activity while you are sore.
RELATED: What Is Focal Hyperhidrosis? 7 Signs of This Chronic Sweating Condition
Laser surgery for hyperhidrosis
Laser surgery is another option for treating armpit sweating. Via tiny incisions in the underarm skin, a laser is passed under the skin to heat up and destroy sweat glands, the IHS explains.
The procedure generally takes less than an hour to complete.
Data on the safety and effectiveness of laser treatment for armpit sweating is limited, consisting mostly of case reports involving a small number of patients, says IHS. A 2018 study in Lasers in Medical Science concludes that large, randomized trials of laser treatment for hyperhidrosis are needed. However, some doctors do offer the treatment.
RELATED: Hyperhidrosis Can Affect Your Feet, Too—Here's What You Can Do About It, According to Dermatologists
Endoscopic thoracic sympathectomy (ETS) surgery
Used to treat severe cases of hyperhidrosis in the palms and underarms, and sometimes in the face, ETS is a major surgery. During this procedure, a surgeon attempts to cut or destroy the nerve paths on the spinal column that are connected to sweat glands in the area of your body you want to stop producing sweat, according to Dr. Glaser.
To locate the nerves to cut, the surgeon inserts a camera through the chest under the armpit. In order to destroy the nerve, your lung has to be temporarily collapsed.
The IHS states that ETS surgery should be considered with great caution and only as a last option when no other treatments provide relief and hyperhidrosis is so severe that it affects a person's ability to live their life.
Dr. Glaser says ETS can cause damaging side effects: "It can cause a major condition called compensatory hyperhidrosis, which can develop six months to 10 years after the surgery." Sweating in the treated area of the body may stop, but profuse sweating begins elsewhere, usually somewhere from the chest down.
"It can be mild, moderate, or severe," says Dr. Glaser. But there's no treatment for compensatory hyperhidrosis—"and it can't be reversed."
ETS can also cause extreme hypotension, arrhythmia, and heat intolerance, and in some cases death, the IHS notes.
While ETS was once a good idea, Dr. Glaser says it has proved to be too dangerous. She has some patients who are happy with the results and others who regret getting the surgery because they developed compensatory hyperhidrosis in the groin area, causing so much sweating that they wear a diaper to cope.
RELATED: Chrissy Teigen Just Got Botox in Her Armpits to Stop Sweating—Here's How That Works
Will insurance pay for hyperhidrosis surgery?
Health insurance organizations often do not recognize surgeries as a treatment for hyperhidrosis, and therefore, usually won't pay for them, says the IHS.
Many patients pay out-of-pocket for these surgeries. But Dr. Friedman says your doctor may be able to help you navigate coverage and cost issues.
To get more stories about health and wellness delivered to your inbox, sign up for the Healthy Living newsletter
]]>Hyperhidrosis is a medical condition that causes an area of the body—or multiple areas—to sweat about four times the amount needed to keep your body temperature regulated, explains the International Hyperhidrosis Society (IHS). When it affects the feet, it's called plantar hyperhidrosis or simply hyperhidrosis of the feet, per IHS.
Wondering whether your foot sweating is over the top? Here's what experts say about this condition and how to treat it.
Who experiences hyperhidrosis of the feet?
The feet are a common site of sweating among people who experience hyperhidrosis.
"Many have multiple areas of sweating; oftentimes hands and feet go together," Dee Anna Glaser, MD, dermatologist at SLUCare Physician Group in St. Louis, tells Health. She says some of her patients have excessive underarm, hand, and feet sweating. And it's not uncommon to sweat profusely in areas such as the groin, buttocks , back, or under the breasts.
Excessive hand and feet sweating often starts very early in life, sometimes as young as 6 months to 1 year, notes Dr. Glaser. "Parents may say their kid 'was always dropping their sippy cup or slipping on the floor, and I always thought they were just clumsy or not coordinated,'" she says.
For people who grow up with hyperhidrosis, the condition can affect their lives personally and professionally. "People who sweat in their hands and feet are often embarrassed to shake people's hands due to sweaty palms or take their shoes off around others. They also might have a hard time with dropping things. I have some patients who are nurses and have a hard time putting in an IV," she says.
Still, many people put off getting treatment.
Adam Friedman, MD, professor of dermatology at George Washington School of Medicine and Health Sciences, says that he often picks up on patients' condition anecdotally during an exam. "I might say, 'I see you're sweating a lot; does that bother you?' and they'll reveal it's something they've dealt with for years," he tells Health. "The patient-reported experience is important with this condition because it impacts their social and personal life in addition to being a physical irritant."
RELATED: What Is Focal Hyperhidrosis? 7 Signs of This Chronic Sweating Condition
What causes hyperhidrosis of the feet?
The exact cause of hyperhidrosis isn't known. But scientists do know what happens when someone has this condition. It all begins with nerves in the body that tell your sweat glands to start sweating, says Dr. Friedman.
Whether triggered by hormones, emotions, physical activity, or brain signals that the body is overheating, the sweat glands overreact and produce excess sweat, says the IHS. So, in the instance of sweaty feet, the nerves are sending messages to the sweat glands in the feet to sweat, yet the feet don't need to sweat as often as they are "told" to stay cool.
While hyperhidrosis tends to run in families, experts say more research is needed to determine which genes are associated with the condition. "I might ask a patient if anyone in his family had sweaty feet, and he'll say, 'now that I think about it, my dad did,'" says Dr. Friedman.
When excessive sweating is caused by an underlying health condition, it's called generalized hyperhidrosis. As the Mayo Clinic points out, this type of hyperhidrosis tends to cause all-over sweating, not limited to a specific body part like the feet. But it is possible in rare cases.
RELATED: What Is Generalized Hyperhidrosis? Experts Explain the Causes of This Type of Profuse Sweating
Does hyperhidrosis cause smelly feet?
People often assume that people who sweat a lot must smell. However, Dr. Glaser says this isn't true. "The way I get people to think about it is if you have a stream of water, it usually doesn't smell. It's when it becomes stagnant and not free flowing that you start to get a little bit of an odor," says Dr. Glaser.
"When [sweat] sits on the skin, the bacteria interact with it and that's what creates the odor. Bacteria like dark, moist places, so having a little bit of moisture may make you more likely to have odor, but people who have hyperhidrosis and have big outbreaks of sweating usually don't," explains Dr. Glaser.
However, Dr. Friedman adds that moisture from excessive sweat on the feet can break down the top layer of skin on your feet, which can cause a change of the structure of the skin. "This allows for pathogens to get in," he says.
Pitted keratolysis, a bacterial infection, can eat away at the top layer of skin. It can become smelly and needs to be treated with antibiotics, says Dr. Friedman. Sweaty feet can also set the stage for dermatophytosis complex, a foot fungus that breaks down the skin, allowing more concerning bacteria to enter the body, he says.
RELATED: What Is Athlete's Foot?—And How Can You Get Rid of It?
How do you treat hyperhidrosis of the feet?
Because the skin on the soles of the feet is thick, Dr. Friedman says it's hard to get medicine to penetrate. However, there are hyperhidrosis feet remedies, such as the following:
Antiperspirants
When applied to the feet, sweat absorbs the antiperspirant, clogging up sweat ducts in the feet. When the ducts are clogged, they send a signal to stop producing sweat. The antiperspirant usually lasts for a day, says the IHS.
Iontophoresis
The IHS says this procedure involves a device that produces a mild electrical current. A person places their feet in a shallow pan of water through which the current passes from the machine through the skin's surface. Weekly treatments can provide long-term benefits.
Botox (onabotulinumtoxin A)
This FDA-approved treatment is indicated for underarm hyperhidrosis; however, some doctors use it for severe cases of hyperhidrosis of the feet, says the IHS. Botox works by temporarily blocking the release of the chemical that initiates the body's sweat glands.
While it can be effective in the feet, Dr. Friedman warns that it should only be given by a qualified doctor who specializes in hyperhidrosis. "The feet can be a sensitive area and Botox can be painful in the feet, so talk with your doctor about your options," he says.
In addition to the treatments mentioned above, there are things you can do to ease the symptoms of plantar hyperhidrosis. Per the IHS:
- Shoe inserts can help absorb sweat and keep you from slipping.
- Powders can absorb moisture and help with slipping.
- Hanging your shoes on a drier as soon as you take them off can help them dry out, so they are ready to wear again.
To get more stories about health and wellness delivered to your inbox, sign up for the Healthy Living newsletter
]]>Don't fret. You might be experiencing psoriasis on your scalp and, yes, there are ways to treat it.
Why do people get scalp psoriasis?
According to the National Psoriasis Foundation (NPF), about 45-56% of people with psoriasis have scalp psoriasis. Additionally, the NPF states that scalp psoriasis is common in people of color.
"We don't know why some people get it on the scalp and some don't," Adam Friedman, MD, professor of dermatology at George Washington School of Medicine and Health Sciences, tells Health.
He explains that while it's not known exactly what causes plaque psoriasis, a combination of genetic makeup and environmental factors are believed to be involved.
While skin cells usually grow and fall off in a month's cycle, the skin cells of those with plaque psoriasis grow faster, due to an overactive immune system. The skin cells tend to grow in about three to four days, yet they don't fall off at the same pace, leaving dead skin cells to buildup on the skin.
While there isn't a known reason for why people get psoriasis on different parts of the body, Dr. Friedman says he finds that those with scalp psoriasis also get inverse psoriasis, which occurs on the folds of skin like the groin and underarms. He notes that because those areas can be moist, psoriasis might look different.
"So, people who have this are often underdiagnosed because it doesn't have that classic appearance. In the groin area, it can be assumed it's a yeast infection or sexually transmitted disease. This is why it's important to make a correct diagnosis," Dr. Friedman says.
Robert T. Brodell, MD, chair of the department of dermatology at the University of Mississippi Medical Center, adds that many of his patients with scalp psoriasis also have it on their elbows and knees, as well as experience pitting in their fingernails.
"I do also have patients with it only the elbows or only the knees or only on the scalp. So, it's a mixed bag," he tells Health.
RELATED: What Is Plaque Psoriasis? How Doctors Diagnose and Treat This Chronic Skin Condition
What are the symptoms of scalp psoriasis?
Symptoms of psoriasis on the scalp might include:
- Fine scaling that looks like dandruff, or appears as thick, crusted plaques on the scalp
- Red, itchy areas on the scalp
- Scaling that covers parts of the scalp or the entire scalp
- Scaling that may extend beyond the hairline onto the neck
"It can be itchy and painful and all that together can make psoriasis that affects a small body area disabling," says Dr. Friedman.
Scalp psoriasis can have a social impact, too, he adds.
"If someone sees a person with a flaky, red scalp, they may assume the person is unkempt or has a fungal infection, so there is an added level of anxiety associated with that in terms of misunderstanding what scalp psoriasis is and punishing the patients," Dr. Friedman says.
RELATED: Psoriasis Causes, Plus 7 Things That Can Cause Symptom Flare-Ups, According to Dermatologists
How does psoriasis affect the scalp and the hair?
Psoriasis on the scalp can sometimes cause hair loss, says the American Academy of Dermatology Association (AAD).
"Even a little inflammation can cause hair loss," Dr. Friedman points out. "Hair is very fickle, it's a prima donna, so to speak; it wants a perfect environment to grow."
Hair is so fickle, he notes, that even dandruff can cause hair loss.
While the AAD says hair often grows back once psoriasis clears on the scalp, it recommends ways to help prevent further hair loss, such as gently combing and brushing away scales, avoiding picking off scales, and letting your hair air dry.
RELATED: Scalp Psoriasis Vs. Dandruff: How to Tell the Difference and What to Do to Relieve Your Scalp Itch
How is scalp psoriasis treated?
There are several options for treating scalp psoriasis, and your dermatologist may use one or a combination of the following to find what works best for you.
Topical ointments
First-line therapy for plaque psoriasis on any part of the body is a topical anti-inflammatory, says Dr. Friedman. The NPF says that topical treatments include medicated shampoos, steroids and tars, and prescription topicals.
"The tricky part is that using an ointment or cream on the scalp can be difficult; think about applying an ointment or cream in a hairy area, that's not easy," he says.
In some cases, he says, foam, liquids, or gels are better options for the scalp. However, he adds that some of his patients who have brittle or dry hair like using ointment on the scalp.
Some topical options are available over-the-counter (OTC). The NPF recommends looking for the following active ingredients:
- Salicylic acid, which softens plaques and scales and removes them from the skin.
- Tar (made from coal or wood), which slows skin cell growth and reduces inflammation, itching, and scaling.
Before buying OTC products, NPF recommends looking at its Seal of Recognition program, which includes products that aim to be non-irritating and safe for people with psoriasis.
Phototherapy
Phototherapy shines ultraviolet (UV) rays on the skin with the intention of slowing skin-cell growth. According to the AAD, it can also suppress an overactive immune system, reduce inflammation, and relieve itchiness so that the skin can heal.
A dermatologist may use a handheld device, which looks much like a blow dryer, to treat scalp psoriasis, says AAD.
The downside of phototherapy? "While it works well, some patients find it hard to go into an office three times a week for light therapy," says Dr. Friedman.
RELATED: Is There a Diet for Psoriasis? 5 Foods That May Be Beneficial and 5 That Probably Aren't
Systemic therapies
If topicals or UV light therapy do not help your scalp psoriasis, your doctor may prescribe medicines or biologics.
There are several types of oral medications that doctors may prescribe to improve psoriasis symptoms. These drugs work by slowing down the immune system and include medicines like methotrexate, apremilast (Otezla) and tofacitinib (Xeljanz), but there are many others, says the NPF.
Biologic medications, which are delivered by injection of IV infusion, target specific parts of the immune system. Again, per the NPF, there are a variety from which to choose, including as adalimumab (Humira), ustekinumab (Stelara), and secukinumab (Cosentyx) and others.
Dr. Friedman often prescribes systemic agents for scalp psoriasis because he finds them more effective than topical options for the scalp and because those with scalp psoriasis have a three-fold increased risk for developing psoriatic arthritis.
"And you're not going to treat arthritis with a topical. But I am quick to have a discussion with patients that when it comes to treatment, it's not one or the other. They can make a good decision based on all the information available," says Dr. Friedman.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>  focal hyperhidrosis that begins early in life and causes excessive sweating from specific, "focal," areas of the body, typically the armpits, hands, feet, and head, says Cleveland Clinic. It's also known as primary hyperhidrosis or primary focal hyperhidrosis.
focal hyperhidrosis that begins early in life and causes excessive sweating from specific, "focal," areas of the body, typically the armpits, hands, feet, and head, says Cleveland Clinic. It's also known as primary hyperhidrosis or primary focal hyperhidrosis.
"By definition, primary focal hyperhidrosis happens for no reason—not from secondary issues," says Adam Friedman, MD, professor of dermatology at George Washington University School of Medicine and Health Sciences in Washington, DC. The sweating should be going on for more than six months, he says.
"I will say most people have had it since childhood but didn't connect the dots," Dr. Friedman tells Health.
Focal hyperhidrosis differs from secondary or generalized hyperhidrosis, a type of excessive sweating triggered by a medical condition or drug that someone is taking.
"Secondary usually comes out of nowhere, and it doesn't stop when you're sleeping. It's important to rule out a medication or other medical condition as the cause of excessive sweating before diagnosing a person with [focal] hyperhidrosis," he says.
If the cause of sweating is due to a medication or an underlying condition, Dr. Friedman says he refers the patient to his or doctor who treats them for that condition.
RELATED: What Is Generalized Hyperhidrosis? Experts Explain the Causes of This Type of Profuse Sweating
What are the symptoms of focal hyperhidrosis?
The American Academy of Dermatology says people with primary focal hyperhidrosis may have excessive sweating:
- In a single area of the body (such as the armpits) or several areas (like some combination of armpits, hands, feet, or forehead)
- On both sides of the body (both feet, for example)
- Soon after waking up
- At least once a week
The back, chest, groin, and under the breasts are also prone to this type of sweating, per the International Hyperhidrosis Society (IHS).
What causes focal hyperhidrosis?
Focal hyperhidosis occurs when sweat glands are overactive, producing too much sweat, notes the Mayo Clinic.
And why does that happen? Cleveland Clinic points out that the condition tends to run in families, so it's possible that there's a genetic component.
How do doctors diagnosis focal hyperhidrosis?
First, your doctor will determine whether your sweating is secondary, which may involve reviewing your medical history and performing certain laboratory tests. Once secondary causes have been ruled out, a primary hyperhidrosis diagnosis may be considered. The IHS states that a dermatologist will take the following into consideration:
A: Age of onset
Focal hyperhidrosis tends to start during childhood or adolescence. Many times, though, people don't seek out help until they have suffered for years, says Dr. Friedman.
"I often ask patients, 'Think back. Were you embarrassed by holding someone's hand or have you always chosen clothes based on whether or not they might show your sweat?' Oftentimes, this helps them realize their condition," Dr. Friedman says.
B: Bilateral sweating
Focal hyperhidrosis typically occurs on both sides of the body, says IHS. For instance, if you experience hyperhidrosis in the underarms, both arms would sweat excessively, not one.
C: Cessation during sleep
When hyperhidrosis is primary, excessive sweating typically stops during sleep. "Oftentimes, if someone is sweating excessively at night, it might be a sign of an underlying condition," says Dr. Friedman.
D: Duration
Assuming your doctor has ruled out secondary causes of hyperhidrosis, duration of symptoms, specifically, two or more episodes of disruptive, extreme sweating per week for the past six-plus months, can serve as another sign of primary hyperhidrosis.
E: Episodes
IHS states that with primary focal hyperhidrosis:
- Sweating doesn't happen constantly
- Sweating episodes vary in frequency, length, and degree
- Sweating is unrelated to the weather, hot conditions, exercise, or stressful situations
Dee Anna Glaser, MD, dermatologist at SLUCare Physician Group in St. Louis explains: "If you are out in a hot, humid summer day at a baseball game, sweating profusely might be [a normal reaction to the weather]. But if you're sitting at a ball game on a non-humid, mid-70-degree day, perhaps sweating profusely is not [typical]." Similarly, gushing sweat while sitting in air conditioning at your desk might indicate hyperhidrosis, she adds.
F: Family
Two-thirds of people with primary hyperhidrosis say that they know family members who also excessively sweat, according to the IHS.
G: Gets in the way
Hyperhidrosis can interfere with your ability to function, participate in social activities, attend outings, and have an impact on mental health.
"For most people, it's a quality-of-life impairment. They're embarrassed at work or at school," says Dr. Glaser. "Some of that can be the discomfort from the physical aspects of having hyperhidrosis, such as having wet underwear from sweating too much from your groin to chaffing under your breast."
She adds that the condition's impact on mental health is serious. "We brought in 300 people with hyperhidrosis and their families, and I heard some patients saying they were considering suicide because of the sweating, which is really terrible. This really affects their quality of life," says Dr. Glaser.
RELATED: What Is Axillary HyperhIdrosis? Causes of Extreme Armpit Sweating—and Possible Solutions
Living with focal hyperhidrosis
Research suggests that 5% of the world's population—hundreds of millions of people—have hyperhidrosis, per the IHS. More people probably have hyperhidrosis but don't realize it or are embarrassed to seek treatment for it, says Dr. Glaser.
"Some teenagers who have underarm sweating say they will never raise their hand in class because they are too embarrassed to show sweat under their arms," she says.
Dermatologists measure quality of life based on 10 domains, such as how a condition is affecting sexual relationships and workability, she says. "We find that people who have hyperhidrosis have impairment among all of them and have some of the worst quality of life scores compared to any other dermatology diseases that we take care of," says Dr. Glazer. It's even worse than severe scaring from acne, psoriasis all over the body, or severe eczema that requires a patient be hospitalized, she says.
While this doesn't mean that hyperidrosis is worse than other skin conditions, Dr. Glazer says it shows that the condition has a bigger impact on a patient's perceived quality of life.
On a positive note, when Dr. Glaser treats patients for focal hyperhidrosis, she says the gains that these patients make in their quality of life are notably better than improvements seen after the treatment of other dermatologic conditions.
RELATED: 8 Hyperhidrosis Treatments to Help People Who Sweat Excessively
How Is focal hyperhidrosis treated?
Various treatments are available for focal hyperhidrosis. The regimen your doctor recommends may depend on the frequency and severity of your symptoms, the body parts affected, and your overall health, notes the Cleveland Clinic.
A 2019 review in the Skin Therapy Letter describes the various options for this type of hyperhidrosis. First-line therapies include antiperspirants and topical wipes. Botox is often next in line, especially for axillary (underarm) hyperhidrosis.
Iontophoresis, a procedure that involves passing a mild electrical current through water into the skin, is considered an effective treatment for people who sweat profusely from hands and feet, the review article notes.
Laser and microwave therapies, oral medications, and surgery are among the other options for treating focal hyperhidrosis. But the first step is to work with your doctor to find the treatment or combination of therapies that works best for you.
To get more stories about health and wellness delivered to your inbox, sign up for the Healthy Living newsletter
]]>While it's necessary to sweat to cool down your body, over-the-top sweating can seriously disrupt a person's daily activities.
Adam Friedman, MD, professor of dermatology at George Washington University School of Medicine and Health Sciences in Washington, DC, explains that excessive sweating is defined as four times the amount of sweat needed to regulate your body temperature.
"We need to sweat. It's our body's natural air conditioning system. However, hyperhidrosis is sweating that is not in response to heat; it's not there to cool you down; rather it's an abnormal amount of sweating for no rhyme or reason," Dr. Friedman tells Health.
For example, he says people with hyperhidrosis may be sitting in an air-conditioned room watching a relaxing movie and experience excessive sweating. "It's too much of a needed good thing. It's well beyond what your body needs to be cool, which is why it is a true medical condition," says Dr. Friedman.
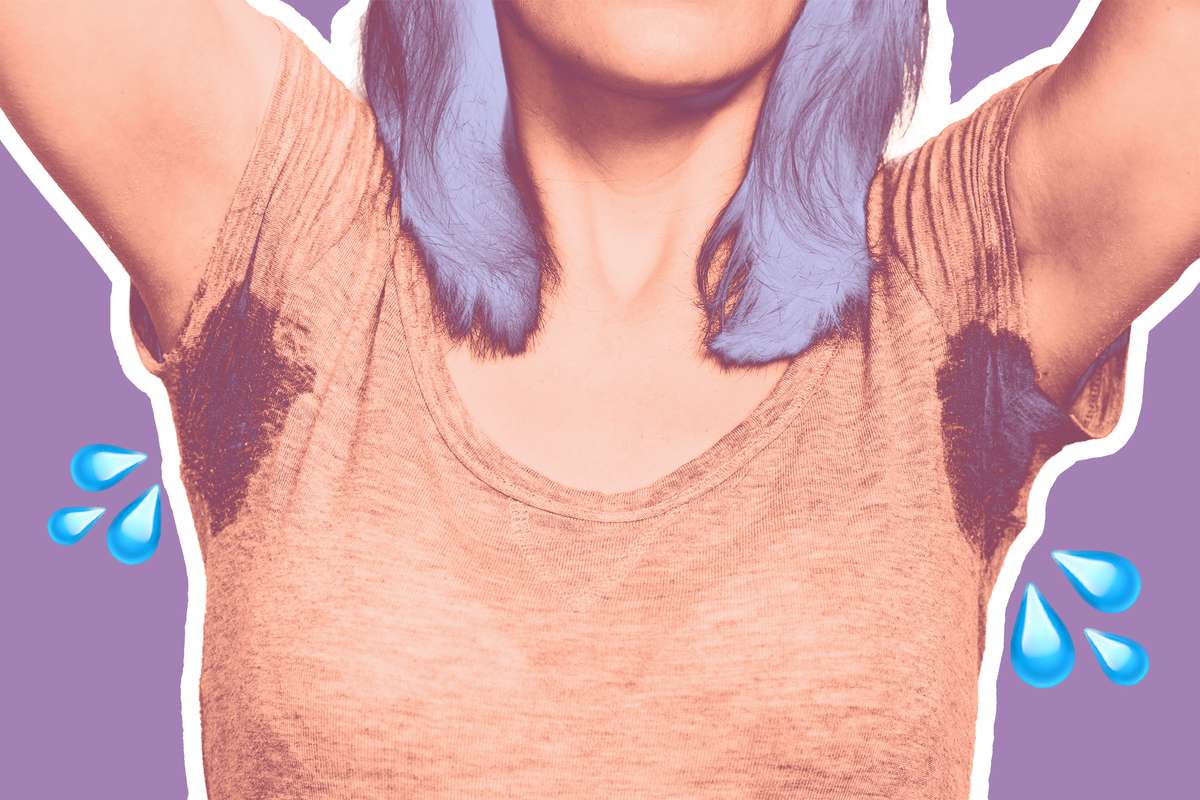 axillary hyperhidrosis , Woman sweating very badly under armpit (IHS), there are between two and four million sweat glands throughout the body, and most are found in the soles of the feet, palms of the hands, forehead and cheeks, and, yes, the armpits (or axillae).
axillary hyperhidrosis , Woman sweating very badly under armpit (IHS), there are between two and four million sweat glands throughout the body, and most are found in the soles of the feet, palms of the hands, forehead and cheeks, and, yes, the armpits (or axillae).
The majority of these glands are "eccrine" sweat glands, which release odorless, clear fluid that help cool the body. The type of sweat produced from the eccrine glands is what most often occurs in hyperhidrosis.
RELATED: Hyperhidrosis Is a Rare Disorder That Causes Me to Sweat Constantly—and I've Finally Learned to Live With It
What is axillary hyperhidrosis—and what causes this condition?
Excessive underarm sweating not caused by another medical condition is referred to as primary axillary hyperhidrosis. While doctors do not know exactly what causes it, they understand how it occurs in the body.
"What's happening is the nerves that sends signals to the sweat glands [which tell them] to sweat are overactive," says Dr. Friedman.
Your sweat glands respond to various stimuli, says the IHS. These include:
- signals from your brain that your body is overheating
- hormones
- emotions
- physical activity or exercise
In people with hyperhidrosis, the sweat glands overreact to these messages by overproducing sweat, says the IHS.
Dr. Friedman notes that hyperhidrosis runs in families, yet scientists have not identified which genes are associated with the condition.
Who develops axillary hyperhidrosis?
Most people with underarm sweating begin experiencing it after puberty, during adolescence or in their early teens, and typically before age 25, says Dee Anna Glaser, MD, dermatologist at SLUCare Physician Group in St. Louis.
"If I have a 60-year old patient who all the sudden starts to sweat all over their underarm, that's not typical of hyperhidrosis, so then we start to think about whether or not something else going on," she tells Health.
While some people who have axillary hyperhidrosis may only have excessive sweating in their underarms, others may have hyperhidrosis that affects other parts of their body, such as the hands, feet, face, scalp, or groin, says the IHS.
Other signs of primary hyperhidrosis include:
- Excessive sweating at least once a week over at least a six-month period
- Sweating on both sides of the body (meaning not just one underarm, but both)
- Sweating so much that it affects your daily activities
When Dr. Glaser is determining a diagnosis, she'll ask the patient if their armpit sweating stops when they sleep. The reason? "People with primary hyperhidrosis don't sweat at night," she says. If someone is sweating profusely from their armpits day and night, that's a sign they don't have primary hyperhidrosis. Their sweating may be due to an underlying medical condition or a drug they't taking—and that's known as secondary or generalized hyperhidrosis.
RELATED: What Is Generalized Hyperhidrosis? Experts Explain the Causes of This Profuse Type of Sweating
Does generalized (aka secondary) hyperhidrosis cause armpit sweating?
Most people who sweat excessively from their armpits have primary hyperhidrosis, but it's also possible for people to develop sweaty armpits due to generalized (aka secondary) hyperhidrosis.
"Both primary and secondary hyperhidrosis can lead to axillary hyperhidrosis," Elizabeth Jones, MD, an assistant professor in the Department of Dermatology and Cutaneous Biology at Thomas Jefferson University Hospital in Philadelphia, tells Health.
With secondary hyperhidrosis, armpit sweating is usually bilateral, says Dr. Jones, "but some people tend to sweat more on one side and so many notice it more in one armpit."
RELATED: Sweat Much? Here's Why and What You Can Do About It
Axillary hyperhidrosis treatment
There are a variety of treatments for axillary hyperhidrosis, per the IHS.
"If you ever hear 'don't worry about it, there's nothing we can do about it, it's not going to kill you,' go get another doctor's opinion," Dr. Glaser advises, because excessive sweating can impact your life socially, emotionally, and physically. She says a dermatologist can work with you to find the best treatment option.
Antiperspirants
Because antiperspirants are the least invasive and are inexpensive, they are often the first type of treatment doctors will use to treat axillary hyperhidrosis, says the IHS. When antiperspirant is applied, the sweat in that area grabs onto it, pulling antiperspirant particles into the pores under the skin. This causes the sweat ducts to "plug," which tells your brain to stop sending messages to sweat in that area.
Botox
Botox (onabotulinumtoxinA) is approved by the US Food and Drug Administration (FDA) to treat primary axillary hyperhidrosis, if antiperspirants are not effective. These injections can temporarily block the release of the chemical that initiates the body's sweat glands. "By blocking, or interrupting, this chemical messenger, botulinum toxin 'turns off' sweating at the area where it has been injected," per the IHS. "Botox injections are very shallow, meaning that the medicine is injected just below the surface of the skin, where it remains."
Laser
While the IHS says the effectiveness of laser treatment for underarm sweating has not been proven in large studies, some doctors do offer it. Lasers can target and destroy sweat glands in the underarm through small incisions. The procedure usually takes less than an hour to complete.
RELATED:8 Hyperhidrosis Treatments to Help People Who Sweat Excessively
miraDry
MiraDry is FDA-approved device to treat axillary hyperhidrosis. It uses microwave technology to destroy sweat glands in the underarm without damaging the skin. Because sweat glands tend to not grow back, the treatment can improve the condition right away, says the IHS. While one treatment is sometimes enough, some people benefit most from a second procedure, three months after the first.
Oral medications
Prescription medications taken by mouth can help stop the sweat glands from producing sweat. Anticholinergics, such as glycopyrrolate, oxybutynin, benztropine, propantheline, are the most common oral medication used for hyperhidrosis, notes the IHS. However, while FDA approved, these medications have not been studied in controlled clinical trials specifically for hyperhidrosis. Still, "dermatologists use off-label medications often," says Dr. Friedman.Just be aware that these medications can cause side effects such as dry mouth, muscle cramps, and urinary retention.
Beta blockers (propranolol) and benzodiazepines are also options for treating excessive sweating. These drugs block sweating that occurs due to anxiety-provoking situations, says the IHS.
Topical wipes
Qbrexza is FDA approved to treat axillary hyperhidrosis. These cloths are used once per day on the underarm and work by blocking receptors that activate sweat glands. The active ingredient is an anticholinergic called glycopyrronium tosylate. Applying this medication topically instead of taking it orally may help reduce side effects, says the IHS.
Underarm surgeries
Underarm surgery can also be an option for treating axillary hyperhidrosis, says the IHS. Common techniques include:
- Excision, which involves cutting out sweat glands.
- Curettage, in which sweat glands are scraped out.
- Liposuction, involves suctioning out sweat glands.
Doctors may use different combinations of each surgery. Because these surgeries permanently remove or damage sweat glands, they can have long-lasting effects. However, sweat glands are very small and often undetectable even with instruments, leaving doctors unaware of how many glands they affected.
There's another option, too. It's called endoscopic thoracic sympathectomy (ETS) surgery, but the IHS cautions that it's invasive and poses serious complications. It involves destroying the nerve paths on the spinal column that are connected to the overactive sweat glands. Most physicians do not recommend it, says the IHS.
To get more stories about health and wellness delivered to your inbox, sign up for the Healthy Living newsletter
]]>But don't confuse it with the most common type of hyperhidrosis, known as primary focal hyperhidrosis. (It's the type that begins early in life and typically affects the armpits, hands, feet, and head, per the Cleveland Clinic.)
So if you're sweating a lot, how can you tell if it's generalized hyperhidrosis—and what can you do about it? We asked dermatologists to explain.
 generalized hyperhidrosis , Water drops on woman skin, close up of wet human skin texture .
generalized hyperhidrosis , Water drops on woman skin, close up of wet human skin texture .
It's also known as secondary hyperhidrosis because it is "secondary" to something else, such as an underlying health condition, explains the International Hyperhidrosis Society (IHS).
As Cleveland Clinic points out, this type of hyperhidrosis tends to affect adults.
What are the symptoms of generalized hyperhidrosis?
One sign that you might be experiencing generalized hyperhidrosis rather than primary is that the sweating doesn't stop when sleeping, says Dee Anna Glaser, MD, dermatologist at SLUCare Physician Group in St. Louis.
In addition, the IHS says people with secondary hyperhidrosis might also experience:
- Sweating on larger or generalized areas of the body
- Onset of excessive sweating in adulthood rather than childhood or adolescence
What causes generalized hyperhidrosis?
There isn't a single cause of generalized hyperhidrosis, the IHS points out. Typically, profuse sweating stems from an illness or underlying health issue or is related to a drug that someone is taking.
Medical conditions
Many different medical conditions can either cause excessive sweating or have sweating as a side effect, per the IHS. Here are just a few:
- Infection or another illness that causes fever
- Alcoholism
- Diabetes
- Gout
- Heart failure
- Hypothyroidism
- Menopause
- Obesity
- Parkinson's disease
- Rheumatoid arthritis
- Pregnancy
- Lymphoma
- Encephalitis
Medicines
A multitude of medications can cause hyperhidrosis—the IHS lists hundreds of "potentially sweat-inducing" prescription and non-prescription drugs.
The IHS and recent review articles published by the US National Library of Medicine (NLM) and in American Family Physician highlight some of the common culprits. They include:
- Tricyclic antidepressants, including desipramine (Norpramin), nortriptyline (Pamelor), and Protriptyline (Vivactil)
- SSRI and SNRI antidepressants, such as fluoxetine (Prozac) and venlafaxine (Effexor)
- Pilocarpine, prescribed for dry mouth
- Zinc supplements (such as Cold-Eeze)
- Insulin
RELATED: Sweat Much? Here's Why and What You Can Do About It
How generalized hyperhidrosis is diagnosed
If you are experiencing excessive sweating, Dr. Glaser says the first step is for your doctor to determine if the sweating is caused by an underlying condition or medication. "This way we can refer them to their doctor who treats that condition or prescribes that medication," she tells Health.
To diagnose the issue, your doctor will likely review your medical history, conduct a physical exam, and ask you about any drugs or supplements you're taking, including over-the-counter medicine and supplements, per the IHS. Two tip-offs that it's generalized hyperhidrosis:
- You sweat when you sleep
- Your sweating came on suddenly during adulthood
If your doctor suspects that your sweating is secondary, laboratory tests may be ordered to rule out potential causes, according to the NLM review.
RELATED: 8 Hyperhidrosis Treatments to Help People Who Sweat Excessively
Generalized hyperhidrosis treatments
If your doctor traces the cause of your excess sweating to a condition that you have or a medicine or supplement you're taking, the solution might be to better manage your condition or switch medications, says Dr. Glaser.
Of course, it's not always possible to control sweating that's caused by an underlying medical condition, notes the American Academy of Family Physicians. And that's where treatments for primary focal hyperhidrosis, the other type of hyperhidrosis,may come into play.
Antiperspirants and topical wipes may help, for example. The IHS also suggests that doctors consider prescribing an oral medicine, such as an anticholinergic drug or beta blocker, to control the sweating.
To get more stories about health and wellness delivered to your inbox, sign up for the Healthy Living newsletter
]]>