I'm no stranger to health issues. At 19, I was diagnosed with ulcerative colitis, an inflammatory bowel disease similar to Crohn's disease that causes diarrhea and abdominal pain. People with ulcerative colitis also have a higher risk of colon cancer because the disease can lead to changes in the colon lining. So I always knew that having my colon removed to prevent the possibility of colon cancer was a strong likelihood.
During a routine colonoscopy when I was 27, my doctor found precancerous changes; he actually said I had one of the worst colons he's ever seen. To prevent those precancerous changes from progressing to cancer, he removed my colon. That required me to live with an ostomy bag—a pouch connected to an opening in my abdomen that collects the waste that would normally be routed through my colon.
After that surgery, I went about my life for several years. I had regular checkups with my gastrointestinal specialist while working as an assignment editor for TV station in Rochester, New York and waitressing or tutoring kids on the side. Seven years later, however, I started feeling pain that would changed my life forever.
A sudden sharp back pain
It was Fall 2014. At my waitressing job, I bent over to pick up a box of bottles for the bar and felt a very sharp, stabbing pain in my back. I chalked it up to getting older (I was now 33) and didn't think much of it. But the pain stayed with me and become progressively worse, evolving into a dull ache I'd feel while sitting, driving, and even trying to sleep. I couldn't sit down comfortably for more than a few minutes at a time. So I visited my primary care doctor to see what was going on.
My doctor had me do lots of stretching exercises and then said she thinks I "pulled a muscle" in my sacrum—the triangular bony structure in the lower back that's also known as the tailbone. It seemed like a really difficult part of the body to hurt, but I accepted her diagnosis. She prescribed me a mild muscle relaxer to ease the constant ache.
That weekend, I was supposed to visit my family two hours away. I said to my mom, "There's no way I can sit in the car for that long." I simply couldn't do it. The muscle relaxer wasn't doing a thing. So I called my doctor's office, telling them I needed something stronger. This was when the opioid crisis was really brewing publicly, and doctors weren't giving out certain pain medications like they used to, which I understood. The nurse I spoke to told me to give the muscle relaxer a little more time. I did make the drive to see my family that weekend and got through it, but I was definitely in a lot of discomfort.
A late-night trip to the ER
A few weeks later, I noticed that I was really altering my behavior to accommodate this pain. When I drove, I would position my body to the side so I wouldn't put a lot of pressure on the right side of my butt and my lower back, where the pain hurt the most. When I sat down in a chair, I would turn a little bit very gingerly. I also tried to lose some weight. The weight loss wasn't drastic, but it seemed like it was coming off easier than in years past. It was also harder to get comfortable at night. I tried to grin and bear it, thinking it was going to get better. Then one night the pain was just raging, so I got up and drove myself to the hospital.
At the ER, they ran a few tests. I was told I had a rectal abscess, where a cavity in my anus became filled with pus. It's a very painful condition that's been linked to ulcerative colitis, and I would need surgery the next day to stop the pain and prevent it from getting larger. Obviously I wasn't happy to hear that, but it sounded like they were on the right path. I was given pain meds to sleep in the ER overnight, and I finally started to feel relief mentally and physically.
The next morning, I had a small surgical procedure where a needle was stuck in my rectum to drain the abscess. My surgeon, who's very well-respected in Rochester, told me the abscess was pretty bad, and it was possible that it could come back. Roughly three weeks later when the pain and discomfort started again, I knew not to wait. I went back to the surgeon for another draining, but the abscess just kept returning. Around the fourth visit, I knew I couldn't go on like this. Toward the end of that visit, my surgeon came in and told me after a more thorough exam that he believes he found a tumor.
News you can’t prepare for
I was shocked, but I also remember saying to him, "I knew it." It all made sense. Everything that I was experiencing crystallized in that moment. He wasn't sure if it was malignant and said I had to wait eight days for the results to come back. It ended up being exactly what I had feared: stage four rectal cancer.
During the eight days I waited for those results, I would tell myself I had cancer. I kept trying that positive diagnosis on, trying to get acclimated and prepare myself fully. I needed to get used to the idea. I felt confident going into that appointment, knowing that I had prepared myself. Yet when my doctor actually said "You have cancer," I remember grabbing the arms of the chair I sat in, feeling like I had been knocked backward. I was not prepared at all. You just can't prepare yourself for that. I don't care if it's a tiny mole or a giant brain tumor, you're just never prepared to hear the words "You have cancer."
RELATED: Doctors Kept Dismissing My Back Pain—Until I Was Finally Diagnosed With Terminal Cancer
I wanted surgery immediately, but it wasn't that simple. My tumor was the size of a softball, and it pressed against a number of nearby organs, including my vagina. I needed chemotherapy and eventually radiation to shrink it down for what would be a major 10-hour surgery to remove what remained. After removing the tumor, a plastic surgeon would have to rebuild my vagina, since getting the tumor out would require taking a part of my vagina. On the bright side, I often joked that I'd have a "million dollar vagina" thanks to cancer.
To make things even worse, I would have to go to a major cancer hospital, like one in New York City or Boston, where I knew no one, because my oncologist said I needed the biggest guns possible to fight this.
Two years of chemo and radiation
I knew my disease was serious, and going through chemo was just the half of it. It left me with cracks all over my feet and made walking painful, so I'd have to bandage and bind them for comfort. It felt like I had paper cuts along my fingernail beds. If I touched something acidic like a tomato, my skin would burn. When I cried, the tears felt like they were burning my face. I had spontaneous nosebleeds without warning. The inside of my mouth became so sensitive that even bland food tasted as if it were covered in hot sauce, like I was chewing razors. In total, I did three round of chemo, which took roughly two years.
Radiation was a lot easier to deal with physically but much more emotionally taxing, as it sent me into early menopause. I started having hot flashes, waking up drenched in sweat with my hair sopping wet. I'd be extremely hot and extremely cold in the same minute. Nobody wanted to ride in a car with me because I was so particular about the temperature. I had to have a hot drink and a cold drink near me constantly. I was emotional all time time. I remember one time seeing a guy driving like an idiot—and I followed him for blocks so I could yell at him! I felt like a hormonal teenager all over again. I spent five weeks going for radiation treatment, including pelvic radiation, which is typical for rectal cancer.
“I’m not going to let this kill me”
By Spring 2016, I'd completed chemo and radiation at different cancer centers between New York and Boston, and I was ready to have the surgery at University of Rochester Medical Center to finally remove the tumor. That's when doctors discovered the cancer had spread to my liver and lungs, and it could no longer be surgically removed. I had gone from finally being in a place to have surgery and move on from cancer. Then with the news that the cancer was inoperable, I was told that there's nothing I can do but try chemo again to try to buy time. To make things worse, my mom passed away that April, a few days before my 35th birthday.
It was really hard losing my mom. Even in my first bout of health issues with ulcerative colitis, my mother was right by side. She'd stay at the hospital with me. She nursed me back to health, all while she was dealing with her own COPD and lung cancer. For a while, we thought we were both going to die at the same time. I would apologize because I was too sick to do anything for her. We were both were useless to one another except for emotional support. Her death added a whole other level of grief.
A novel cancer treatment
Back in Rochester, I underwent genetic testing for my cancer. No genetic link was found, meaning this type of cancer didn't run in my family. I also went for genomic testing, through Foundation Medicine, looking at mutations in the tumor itself. That's when my oncologist suggested I try immunotherapy, a type of cancer treatment that works with your immune system to fight off the cancer.
Immunotherapy was still new at the time, and I didn't really know anything about it. I asked what would happen if I don't do it, and my oncologist said I would have at most two months to live, which rattled me to my core. I kept telling my doctors 'This cancer is not going to kill me, I'm not going to let this kill me," so I had to do everything I could to make that come true.
RELATED: This Woman's 'Gluten Intolerance' Turned Out to Be Uterine Cancer
My immunotherapy treatment involved a short infusion, similar to chemo. It had very few side effects; they were similar to that of the flu. It was easy, actually. The treatment worked so well that the tumors shrunk—especially the rectal tumor. We saw results in two weeks. One year consisting of two immunotherapy treatments have extended my life.
Now my doctors encourage me to see my cancer as more of a chronic illness instead of a death sentence. I outlived the initial predictions. Once I got to my five-year point, my tumors had shrunk so much that I'm able to live with them. I felt such a sigh of relief. I'm 40 now, an age I didn't think I'd live to see. Since the five-year survival rate of stage four rectal cancer is abysmal, my goal was just to get to 40. Now I feel so cautiously optimistic that I'll make another decade at least.
Life with cancer
Aside from having cancer, losing my fertility to pelvic radiation is something I still wrestle with. That has been the most painful thing, honestly. I said I would do anything to fight my cancer, but I always wanted to be a mother and didn't want to jeopardize that. I wanted to freeze my eggs, but my team said I simply didn't have time; I couldn't delay treatment and had to start immediately. Taking away my chance to be a mother was the cruelest thing cancer did.
However, immunotherapy gave me back my life. I started working full-time again after four to five years dealing with cancer. I have two young nephews that I help take care of, sometimes for a whole weekend. I'm not who I was before cancer, but I'm the best I've been since cancer.
Right now, my cancer feels far in the background. I know the tumors are still there, but they've remained shrunken. I would love for them to be gone, but I don't know if it's going to happen, so I just live with it. I haven't had to have any immunotherapy treatments since Winter 2017. My doctor gets more and more confident after my regular scans, telling me my life is being extended more and more.
RELATED: This Woman's Searing Toothache Was Misdiagnosed by Doctors, and It Turned Out to Be Cancer
I don't like to think my primary care doctor made a mistake when she diagnosed a pulled muscle. I still see her and I trust her, because she did the best she could with what she knew at the time. Most people wouldn't conclude that back pain is cancer. When she found out about my diagnosis, she called to apologize to me, telling me how bad she felt that I was going through this, offering up anything she could do. She was also my mother's doctor, and she encouraged me to fight like her. I give her a lot of credit for that.
Because I had health issues at a young age, I've always been grateful for the good things in life, so I really don't take things for granted. I don't make the most of every single second, but I surely make the most out of more of them than ever before. Now I'm happy just to hear a bird tweet simply because I can hear it. I'm elated when the sun shines. Even on bad days I'm mostly happy, because I'm alive to have had that bad day.
To anyone suffering from mystery symptoms and looking for the correct diagnosis, you are your own best advocate; you have to listen to yourself if something is nagging you or doesn't feel right. Speak up, because no one else is going to do it for you. You're not being selfish if you fight for yourself. Keep making noise until you feel like your needs are being addressed.
If you have a story to share about being misdiagnosed, email us at misdiagnosed@health.com and join our Misdiagnosed Facebook community to talk to women who share the same struggle.
]]>Conversely, in the over-50 crowd, the diagnosis rates of colorectal cancer have actually decreased, thanks in large part to more people getting the recommended screening tests to find the disease at its earliest stages—a huge factor in whether or not someone will survive a colorectal cancer diagnosis.
 TK-Colorectal-Treatment-Options-GettyImages-520971055 , MD, a colon cancer surgeon and director of the Johns Hopkins Kimmel Cancer Center for the National Capital Region, tells Health. "The treatments are really changing and evolving and very much individualized to the patient."
TK-Colorectal-Treatment-Options-GettyImages-520971055 , MD, a colon cancer surgeon and director of the Johns Hopkins Kimmel Cancer Center for the National Capital Region, tells Health. "The treatments are really changing and evolving and very much individualized to the patient."
In that case, each specialist might suggest a different method of treatment and, often, they'll work together to attack the cancer through multiple types of treatment. Here's what you need to know about each type of colorectal cancer treatment available, and when they're most likely to be used.
What is colorectal cancer?
First, a recap: Colorectal cancer, like any cancer, begins from changes in one cell or a small group of cells in the body. "Cancer is an uncontrolled growth of a certain cell type and can be found in any tissue in your body," Richard Whelan, MD, chief of colon and rectal surgery at Northwell Health, tells Health.
Colon and rectal cancers are found in the digestive system. The colon is the main part of a person's large intestine and stretches nearly five feet long. The rectum is a section of tissue only a few inches long at the end of the large intestine.
What's different about colorectal cancers is that they grow out of polyps, which are small bundles of tissue that bulge out of the organ itself. "There's this normal progression from the normal, to the polyp, to a scary looking polyp or what we would call "high grade dysplasia" which is kind of pre-cancer, and then turning into a cancer," Dr. Rajput says.
Colorectal cancer is extremely preventable if the polyps are caught early. But if they aren't, they can puncture the intestine, causing bleeding or obstruction of the waste moving through the digestive tract, and travel from the colon or rectum to other parts of the body. Typically, colorectal cancer that spreads goes to the liver or the lungs, but once the cancer gets into the bloodstream or the lymphatic system (a network of tissues, vessels, and organs), it can spread anywhere. When it spreads, doctors classify it as metastatic colorectal cancer.
RELATED: What Is a Colonoscopy? From Prep to Recovery, Everything you Need to Know About the Procedure
How is colorectal cancer treated?
According to Dr. Rajput, there are three main ways colorectal cancer are treated: surgery, chemotherapy, and radiation. The National Institutes of Health classify seven different types of colorectal treatments overall, adding four more treatment options as offshoot treatments in addition to the main three: radiofrequency ablation, cryosurgery, targeted therapy, and immunotherapy—all offered depending on the stage of a patient's cancer.
Surgery
More often than not, colorectal cancer treatment will include surgery, Dr. Whelan says. "The vast majority of patients are treated by taking out a piece of the large bowel, and then the surgeon will try to put the two pieces back together," he says.
How invasive the surgery is depends on the stage the cancer is in. If colorectal cancer is caught in early stages, a surgeon may take out only a small amount of the colon through a process called local excision, according to the NIH. During a local incision, the surgeon will likely get to the colon through the rectum, putting a tube that includes a cutting tool up through the rectum so that they don't have to cut through the abdominal wall. After a local incision, doctors will follow the patient very carefully to ensure the cancer doesn't come back, Dr. Rajput says.
If the cancer isn't caught until later stages, the surgeon will perform what's called a partial colectomy, meaning that they'll cut out the cancerous portion of the colon as well as a small amount of healthy tissue around it. Usually, the doctor will also take out lymph nodes near the colon in order to test whether the cancer has metastasized.
In most cases, colon resections don't cause problems with the function of the bowel later. If they have to take out a section of the colon, surgeons will perform an anastomosis, meaning that they'll sew the two remaining, healthy parts of the colon together. The remainder of the colon then makes up for what was taken out, Dr. Rajput says. "So, most of the time you don't have to worry about getting a colostomy bag, although those are usually temporary, he says.
A colostomy bag is a bag placed around an opening surgeons make on the outside of the body (called a stoma) so that digestive waste can pass outside of the body if the two healthy sections of colon can't be sewn together. In emergency colon surgeries, a temporary bag may be used to allow the colon to heal. However, if the doctor needs to remove the entirety of the lower colon, the bag may be permanent.
Permanent colostomy bags are more common when the colorectal cancer is found in the rectum, Dr. Rajput says. "I often say that it's like real estate, it's 'location, location, location'," he says.
When patients have cancer very low in the rectum or cancer that involves the sphincter complex — which includes a ring of muscle that controls bowel movements — surgeons have to remove the sphincter in order to get control of the tumor. Without a sphincter, a person couldn't control when they poop and so surgeons will attach a permanent colostomy bag to collect waste.
Chemotherapy
Sometimes, chemotherapy can be used on its own to treat colorectal cancer, but it's often used in combination with surgery, Dr. Whelan says. "The general trend is that if you've got metastatic disease that you cannot remove entirely, you rely on chemotherapy primarily before you do surgery," he says.
Chemotherapy uses drugs to stop cancer cells from growing, either by killing them or by stopping them from dividing, according to the NIH. Chemotherapy drugs can be taken by mouth or by an injection (known as systemic chemotherapy), or by an oncologist who will target the drugs directly to a specific area of the body (known as regional chemotherapy).
Often, doctors will suggest chemotherapy for patients who have cancer low in the rectum in an attempt to save the rectum and avoid a colostomy bag. "What we're finding with rectal preservation is that there's a subset of patients who have an excellent response with chemotherapy and radiation and we don't find any evidence of tumor when they come back," Dr. Rajput says. Then, the doctor will do something called "watchful waiting," essentially keeping a close eye on the cancer in case it comes back.
At times, chemotherapy will also be used after surgery as a way to ensure any leftover cancer cells are killed before they can spread. "It's a very small subset of these cells that can set up shop elsewhere, but that's what we're trying to kill," Dr. Rajput says.
RELATED: 12 Colorectal Cancer Risk Factors to Know About
Radiation therapy
The treatment options for rectal cancer are a little different than those offered for colon cancer, Dr. Rajput says, and that's mostly because rectal cancer treatment includes radiation therapy.
Radiation therapy uses high-energy x-rays or other radiation to kill cancer cells or stop them from growing, according to the NIH. Radiation therapy can be either internal or external. Interal radiation is given through a radioactive substance concealed inside needles, seeds, wires, or catheters that a doctor will place directly into or near the cancer. External radiation uses a machine to send x-rays or other radiation toward the cancerous area of the body.
Typically, external radiation is used as a palliative therapy once cancer has reached an incurable stage in order to help patients feel better. Internal, targeted radiation is used to kill the cancer from the inside and, as Dr. Rajput said, is often used in combination with chemotherapy.
Radiofrequency ablation
Radiofrequency ablation isn't used to treat the primary tumor, Dr. Rajput says. Instead, it can sometimes be used to treat colorectal metastases, which are tumors or abnormal cell growth in areas where the primary cancer has spread to.
During radiofrequency ablation, doctors will use a probe that has tiny electrodes that kill cancer cells through electrical energy and heat, according to the NIH. A radiologist will insert the probe directly through the skin or through an incision in the abdomen, using imaging technology to guide a thin needle into the cancer tissue.
Because it's so targeted, radiofrequency ablation is typically used to treat just one (usually particularly difficult) spot of cancer rather than the cancer as a whole, according to the Mayo Clinic.
Cryosurgery
Like with radiofrequency ablation, cryosurgery is a directed treatment used to destroy one tumor rather than treating the cancer overall. Cryosurgery uses a "cryoprobe" — a hollow instrument that circulates very cold gas such as liquid nitrogen or argon gas, according to the NIH. During the procedure, a doctor will use an ultrasound or MRI to guide the cryoprobe to the tumor. Once it touches the tumor, the cryoprobe forms a ball of ice that freezes the tissue, killing the cancer cells. After the cryosurgery, the frozen tissue will thaw and be absorbed by the body.
Cryosurgery is also used externally to treat tumors that have grown on the outside of the body, like those on the skin. For external cryotherapy, liquid nitrogen is applied directly to the tumor with a cotton swab or a spray, according to the NIH.
Targeted therapy
Targeted therapy falls under the broad category of chemotherapy, Dr. Rajput says. Medical oncologists will use targeted therapy to identify and attack specific cancer cells. "Targeted therapy uses newer drugs that target receptors or signaling pathways that are critical for tumor growth," Dr. Rajput says.
There are two types of targeted therapies used to treat colon cancer, according to the NIH. One, called monoclonal antibodies, are lab-made immune system proteins that can attach to cancer cells or cells that help cancer grow and then kill the cells, block their growth, or keep them from spreading.
The other, called angiogenesis inhibitors, stops new blood vessels from growing in the tumor, which stops the tumor itself from growing.
Immunotherapy
Immunotherapy is also part of medical oncologists' toolbag in treating colorectal cancer, Dr. Rajput says. As it implies, immunotherapy uses the patient's immune system to fight cancer. Medical oncologists will use substances, such as certain proteins, made either in the body or in the lab to boost, direct, or restore the body's immune system in hopes that it will target the invading cancer cells, according to the NIH.
Though these treatment options can give anyone diagnosed with colorectal cancer a great fighting chance against the it, the best offense against the disease is still a good defense. That means scheduling and sticking to the recommended colorectal cancer screenings starting at age 45, like having a colonoscopy every 10 years, for those without an increased risk of the disease. Colorectal cancer is largely preventable, Dr. Rajput says, and while the screenings for the disease can seem off-putting at first, they can (and do) save lives.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>Think you’re too young to worry? “We’re seeing more people in their 30s and 40s, including younger women who are the picture of health, being diagnosed not just with [colon] cancer but advanced cancer,” says Dr. Kahi. In fact, an estimated 49 people under 50 will be diagnosed every day this year with what’s known as early-onset colorectal cancer. Here’s what you need to know about the test, including why you might need one sooner than you think.
RELATED: 12 Colorectal Cancer Risk Factors to Know About
The Prep
The key to a successful colonoscopy is making sure your doctor can get a good look at every inch of your colon—and that means drinking a laxative solution and following certain dietary restrictions to get your insides squeaky-clean. The process has a bad rap, thanks in part to a foul-tasting liquid that is no longer used. The new drinks taste better, you don’t have to drink as much, and you typically can drink the laxative in two sessions.
The prep process may start five to seven days before the procedure, so be sure to read the instructions ahead of time, says Natalie Cosgrove, MD, an assistant professor of medicine at the Washington University School of Medicine in St. Louis. One of the most common mistakes patients make is waiting until the last minute to read the prep instructions—at which point they may realize they’ve done something wrong and need to reschedule the test, she says.
RELATED: When Should I Start Colorectal Cancer Screening?
Not every hospital or doctor recommends the exact same approach, so read your doctor’s guidelines at least 10 days before your procedure—and follow them carefully. She’ll most likely recommend that you stop taking over-the-counter fiber supplements and antidiarrheal medicines and supplements containing iron and vitamin E and stay away from high-fiber, slow-to-digest foods that might linger in the colon (like beans, seeds, multigrain bread, salad, vegetables, and fresh or dried fruit) several days to a week before the colonoscopy. She’ll also recommend that you arrange for a friend or family member to pick you up after the procedure since you’ll be having anesthesia or some type of sedation.
The day before the procedure, you can’t eat solid food or consume alcohol, but you should drink enough clear liquid—like water, apple or white grape juice, broth, and coffee or tea (without milk or creamer)—to stay hydrated. And you’ll probably start drinking the laxative at 6 p.m . It works by drawing water into your intestines, triggering numerous watery bowel movements. You’re going to go a lot, so don’t leave home. (The solution also contains electrolytes to prevent dehydration.) At some point, the stuff coming out is going to look clear, but don’t stop drinking until the solution is all finished. “Patients think they’re good to go when they’re having clear diarrhea, but there may [still] be fecal matter left in your colon. You have to drink all of it unless your doctor tells you it’s OK to stop,” says Dr. Cosgrove. You should refrain from eating or drinking anything two hours before the procedure.
RELATED: Single Mom of 3 Vows to Fight After Colon Cancer Spreads Throughout Her Body: 'My Kids Need Me'
The Test
The whole process—checking in for the procedure, meeting with the anesthesiologist or doctor, and getting an IV placed—can last a couple of hours, but the procedure itself usually takes between 20 and 30 minutes, or sometimes longer, if you have polyps that need to be removed. During the procedure, your doctor uses a long, thin, flexible tube with a camera at the end to examine your colon. To remove most polyps, she may use a contractible wire loop to encircle them, severing them from the colon wall. Sometimes an electric current is used with the wire, depending on the size of the polyp. “Most people come out of anesthesia and don’t even realize they’ve already had the procedure,” says Dr. Kahi.
You may feel crampy afterward because the doctor pumps air into your colon to see the tissue more clearly. But serious complications are rare. Three of every 10,000 procedures result in a punctured colon, and eight of 10,000 tests that include polyp removal cause bleeding—problems that are almost always treated promptly and effectively, says Dr. Kahi. Because of the anesthesia, you’ll be a little foggy for the rest of the day, so you shouldn’t try to work or make any big decisions. You’ll be hungry, too, but stick with easy-to-digest foods, like scrambled eggs, applesauce, or well-cooked vegetables. And drink plenty of water and broth or a sports drink to restore fluids and electrolytes.
RELATED: The Colorectal Cancer Symptoms You Need to Know, Even If You're Young
New Thinking on Screening
In response to the early-onset trend, the American Cancer Society revised its guidelines in 2018 to say that everyone should get screened for colon cancer, through either a colonoscopy or a stool-based test, at age 45—five years earlier than previously recommended.
Not all doctors or medical organizations agree with the change. “We end up doing a lot of screening and [proportionately] don’t find that many cancers,” says Dr. Kahi. (The American Gastroenterological Association recommends that average-risk people start screening at age 50.) So talk to your doctor about what’s best for you. She may want to begin screenings at 45 if you have any lifestyle-related risk factors associated with colon cancer—if you smoke or drink, for instance, or you’re inactive or you eat a low-fiber, high-fat diet. She’ll want to know if there is a family history of colon cancer or polyps. “If you have a first-degree relative who had colon cancer, start screening 10 years before the age that the relative was diagnosed or when you are 40, whichever is earlier,” says Jennifer Maratt, MD, a gastroenterologist and assistant professor of medicine at Indiana University School of Medicine in Indianapolis. Because African Americans are at an increased risk for early-onset colon cancer, the American College of Gastroenterology suggests they begin screening at age 45.
And, at any age, if you have blood in your poop, ask your doctor for a test. “It used to be that we didn’t worry greatly about bright red blood in a young person because it is often associated with hemorrhoids. Given the increasing incidence of colon cancer in younger people, however, we’ve become more vigilant, offering a colonoscopy to anyone who experiences bleeding, regardless of the color of the blood,” says Dr. Kahi. Other possible colon cancer symptoms you should bring to your doctor’s attention: persistent abdominal discomfort or pain, or changes in the consistency of your stool. But everyone with a colon has a risk of developing colon cancer, says Dr. Kahi: “Everyone should be screened at 50 at the latest.”
RELATED: I Went to the Doctor With Stomach Pains—and Found Out I Had Stage 4 Colon Cancer
Your sedation options
When Stephanie Bell, of Lexington, Kentucky, had a colonoscopy at 52, she chose an option few people even know exists: no sedation at all. “My fiancé had recently undergone the procedure without sedation and said it didn’t hurt. I don’t like to get IVs, anesthesia upsets my stomach, and I didn’t want to be groggy afterward because I wanted to go to a party later that day. So I decided to try it too,” she says. “My doctor talked to me throughout the procedure and warned me when I might feel a little discomfort because the scope had to make a turn in my colon. I felt pressure, like a Pap smear, but it wasn’t painful. The embarrassment of having a tube inserted and seeing my colon on video was the worst part. But I would definitely do it again.”
Dr. Kahi says the majority of his patients who go sedation-free are enthusiastic about the approach. Because you don’t need an IV or medication, the procedure is less expensive than sedated colonoscopies. Another plus: You can drive yourself home afterward and do not have the same restrictions as someone who received sedation. But Dr. Kahi estimates that only a minority of patients choose it. “Most patients don’t want to be aware [of what’s happening] or feel any discomfort,” he says. If you’re one of them, here are the other two common approaches:
Moderate sedation (aka Conscious sedation or twilight sleep)
A doctor or nurse administers two medications, often midazolam, a benzodiazepine sedative that helps you relax, and fentanyl, an opioid to numb the pain. Because the drugs don’t knock you out, you might be aware of what’s happening during the procedure, but thanks to the amnesiac properties of midazolam, you’re unlikely to remember it afterward. It takes time for the drugs to clear from your system, so you’ll need to lie low for the rest of the day.
RELATED: This At-Home Stool Test Is Just as Effective as a Colonoscopy
Deep sedation (aka monitored anesthesia care)
An anesthesiologist administers a drug, usually propofol, and monitors you during the procedure, which makes it more expensive. The drug doesn’t numb pain, but you’re sedated enough that you should be completely unaware of what’s going on. (Deep sedation differs from general anesthesia, in which you’re intubated with a breathing tube and a machine breathes for you; this is very rarely needed for a colonoscopy.) It causes less residual grogginess than moderate sedation, though you still need a ride home.
Do-it-yourself testing
If you don’t have worrisome symptoms or lifestyle or genetic risk factors for colon cancer, there’s a simpler test that doesn’t involve days of prep or any downtime and is usually covered by health insurance. Known as Cologuard, all it requires is a small poop sample (you can get the testing kit from your doctor or online through a telemedicine provider), which you mail to a lab, so technicians can check for blood as well as changes in your cells’ DNA associated with colon cancer or precancer. If the test is positive, you’ll need a colonoscopy. If it doesn’t find anything, you can wait three years before repeating it. But be aware that the test isn’t as effective as a colonoscopy. A clinical study of nearly 10,000 people published in 2014 in The New England Journal of Medicine found that Cologuard detected 92 percent of the cancers that were found by colonoscopy and just 42 percent of suspicious polyps. So if you develop any symptoms—bleeding, stool changes, bloating, or unexplained weight loss—ask your doctor about having a colonoscopy, even if you’ve had a negative stool test, says Dr. Kahi.
This article originally appeared in the September 2020 issue of Health Magazine. Click here to subscribe today!
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>This made it even more devastating when Boseman’s family revealed his death. On August 29, a statement on the star’s Twitter page described him as “a true fighter” and “a global icon and an inspiring symbol of Black power.”
Boseman was only 43 when he died, and his death brings an important issue to light: that rates of colon (colorectal) cancer are higher among younger Black men. Rates of colon cancer are 30% higher in men than in women of all races. And Black people have the highest rates of colon cancer of any racial or ethnic group in the US, according to the American Cancer Society (ACS).
During a four-year span from 2012-2016, colorectal cancer incidence rates in Black people were about 20% higher than those in non-Hispanic whites (NHWs) and 50% higher than those in Asian/Pacific Islanders (APIs). Mortality is higher too. Colon cancer death rates in Black people are almost 40% higher than the rates for NHWs and double the rates for APIs.
RELATED: 12 Colorectal Cancer Risk Factors to Know About
While the overall numbers for colon cancer are going down, the instances of it in men under 50 are actually going up. In 2017, a large study of invasive colorectal cancers, funded by the ACS and published in the Journal of the National Cancer Institute, found that people born around 1990 have double the risk of developing colon cancer and quadruple the risk of developing rectal cancer compared with those born around 1950. This prompted the ACS to lower its recommended screening age for colorectal cancers from 50 to 45.
Why are colon cancer rates disproportionately high in younger Black people?
Experts don’t really understand why colorectal cases in younger people are rising, Mark Pochapin, MD, director of gastroenterology at NYU Langone Health and president of the American College of Gastroenterology, tells Health. “The rates are going up by 2% per year, though the rates of occurrence are still nowhere near as high for people who are over the age of 65.” Some believe it might have to do with a change in the microbiome, which is the bacteria in the gut, from either using antibiotics or other environmental factors experts aren’t aware of, he adds.
The higher incidence in Black people is also difficult to explain. “This in part may be due to socioeconomics and access to health care, but there may be other factors that we just do not understand,” he says.
Stacey Cohen, MD, a physician at Seattle Cancer Care Alliance and an associate professor in the division of medical oncology at University of Washington School of Medicine, believes that the high incidence and mortality rates in Black patients are due in part to the systemic racism that prevents earlier recognition of a medical condition.
“Colorectal cancer is thought of as a disease for older individuals, and so the diagnosis may be missed for months or years in a younger person,” adds Dr. Cohen. “Cancer is also difficult to detect at an early stage if a provider is not specifically evaluating for it.”
RELATED: The Colorectal Cancer Symptoms You Need to Know, Even if You're Young
What are the warning signs of colon cancer?
In the very early stages, colon cancer typically doesn’t present any symptoms, because the tumor is small and causes no discomfort. “It can bleed as it grows, so people may see blood in their stool,” says Dr. Pochapin. “Additionally, the tumor can start to obstruct the opening of the colon, which can cause narrowing of the stool, making it look pencil-thin, or even cause difficulty passing it. Further, cancer can cause the development of pain and unexplained weight loss. There may also be unexplained anemia on a blood test that is caused by the chronic loss of blood.”
Are there other risk factors for colon cancer?
People with inflammatory bowel disease (IBD) are at higher risk for developing colon cancer, says Dr. Cohen. “There are some hereditary conditions that increase an individual’s risk, and a family history of colorectal cancer or precancerous polyps also increases an individual’s likelihood of developing cancer themselves," she adds.
Lifestyle factors that may increase the risk of colorectal cancers include a diet high in red meat and alcohol consumption, and low in fiber.
“However, these factors do not predict or explain every case,” says Dr. Cohen. “This is why the number one thing we recommend is to undergo age-appropriate colorectal cancer screening and to discuss any concerning symptoms with your doctor.”
RELATED: What Is a Colonoscopy? From Prep to Recovery, Everything You Need to Know About the Procedure
What colorectal screening tests are available?
Multiple screening tests are available for colorectal cancer. “The two most common are colonoscopy and something called ‘fecal immunochemical testing’ (FIT),” says Dr. Pochapin.
A colonoscopy is a test done after a bowel prep, where you take a laxative to clean out the colon the night before. The next day, at a doctor’s office, procedure area, or hospital, a scope or instrument is inserted into the rectum while the patient is under sedation.
“This travels through the colon looking for polyps," explains Dr. Pochapin, which are precancerous growths. “During the procedure we remove any that are found, so it is both diagnostic and also therapeutic—by removing the polyps we prevent the cancer. Of course colonoscopy also looks for early cancer, but the main purpose is prevention.”
FIT testing, on the other hand, is done at home, using a stick or small paintbrush to put a stool sample on a little card. This is sent to the lab to look for microscopic amounts of blood.
“The concept here is that with early cancer, you will find trace amounts of blood in the sample,” says Dr. Pochapin. “If a FIT test is positive, the patient must get a colonoscopy relatively soon to make sure there isn’t a cancer causing the positive test. FIT testing looks for an early cancer, since it isn’t very good at finding polyps, and that’s why it’s more of a cancer detection test than a cancer prevention test, like colonoscopy.”
RELATED: What Are Health Disparities? Why It's Important to Fight for Health Equity—Especially Right Now
Other tests include Cologuard, another type of stool test, which detects abnormal DNA, and virtual colonoscopy, which is performed with a CAT scan.
At what age should I start colorectal cancer screening?
People who have a family history of colon cancer generally start testing 10 years earlier than the age at which the youngest person in the family who had cancer was diagnosed, says Dr. Pochapin. But it’s important to discuss that with your medical team because if there is clustering of family cancers, you may need to get genetically tested. Otherwise, he says everybody over age 50 should start screening. (But discuss with your doctor if you want to be screened earlier, because the ACS does recommend age 45.)
“Black people should start screening at age 45 due to the higher incidence and higher mortality,” suggests Dr. Pochapin. “And if you already have symptoms, such as rectal bleeding, that’s no longer considered ‘screening’ but rather diagnostic. It’s very important to see a doctor to figure out why it’s happening.”
If you’re younger than the recommended screening age but you have symptoms, then speak up. “Please advocate for yourself,” says Dr. Cohen. “If something doesn’t feel right for your body, discuss with your primary care provider whether a diagnostic colonoscopy should be done.”
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>The patient, a 59-year-old man with metastatic colon cancer, presented to the clinic following 10 weeks of experiencing painless, nonpruritic (not itchy) skin lesions that had formed around a large abdominal scar from a previous procedure to remove part of the man's colon three years earlier. The same incision had been used to perform a liver resection and a cholecystectomy (removal of the gall bladder), following the initial procedure.
According to the case report, "on examination, the lesions were firm, pink to violaceous [violet] in color, and vesicular-appearing." The man also presented with ascites, or abnormal buildup of fluid in the abdomen. Following a skin biopsy, doctors confirmed that the man's colon cancer had metastasized to his skin, and the patient was diagnosed with metastatic colon adenocarcinoma.
RELATED: This Man Died After Developing Huge Lesions on His Skin From Rectal Cancer
The occurrence of cancer spreading from a person’s internal organs to their skin—known as cutaneous metastasis—is rare, but it happens in 4–6% of colorectal cancer cases, according to Eric Johnson, MD, a colorectal surgeon at Cleveland Clinic. “It’s something you don’t see very often, [but] it can happen,” Dr. Johnson tells Health. More data, from a 2017 case report published in the Annals of Surgical Treatment and Research, puts the occurrence rate of cutaneous metastases resulting from colorectal adenocarcinoma at more like 3% of colorectal cancer cases.
Overall, the spread of cancer—referred to as metastasis—can happen through a series of steps, according to the National Cancer Institute (NCI). Initially, cancerous cells can grow into or invade nearby normal tissue. From there, those cells can move through the walls of nearby lymph nodes or blood vessels, where they can begin traveling through the lymphatic system and blood stream to other parts of the body. At any point in that process, those cancerous cells can stop at another location in the body, where they can form a tiny tumor and cause new blood cells to grow to create a blood supply for that new tumor.
RELATED: What Is Corkscrew Esophagus? Here’s What a Gastroenterologist Says
But Dr. Johnson says the man in the NEJM case report experienced a different type of metastasis—specifically through tumor cells' contact with the man's outside skin. “If you operate on a colon cancer patient, you’re extracting the tumor. You can shed tumor cells that can implant [in the skin]," says Dr. Johnson. This is why, according to the NEJM case report, "the most common site of cutaneous metastases in colon adenocarcinoma is the abdominal skin, sometimes in or around surgical scars, as was seen in this case." The 2017 case study also explains that cutaneous metastases in colon cancer "generally occur within the first two years after resection of the primary colorectal tumor."
To prevent this spread, surgeons often use devices called wound protectors, which are put in place around wound openings during surgery to keep cancer from spreading from an organ to an incision. “They’re basically a thin, vinyl sleeve that is sterile,” Dr. Johnson explains. While most surgeons use these wound protectors, they aren’t used in every operation, says Dr. Johnson. He goes on to say that this could have been the reason the patient featured in the NEJM report developed the lesions on his stomach, which had spread from his colon cancer, but without a full patient history, nothing can be said for sure.
Unfortunately, the man featured in the NEJM case report received hospice care following his diagnosis but passed away five months presenting to the dermatology clinic.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>The patient had a type of rectal cancer called mucinous adenocarcinoma, which is when a tumor is comprised in part by mucin, a compound found in mucus. His cancer was originally treated with a surgery called a laparoscopic abdominoperineal resection. This procedure is used to treat cancers in the anus and rectum that are close to the sphincter muscles, and it involves removing the anus, rectum, and part of the large intestine through multiple small incisions.
Two chemotherapy drugs—capecitabine and oxaliplatin—were recommended after surgery for this patient, according to the case report, but he decided against taking these medications, which can be expensive.
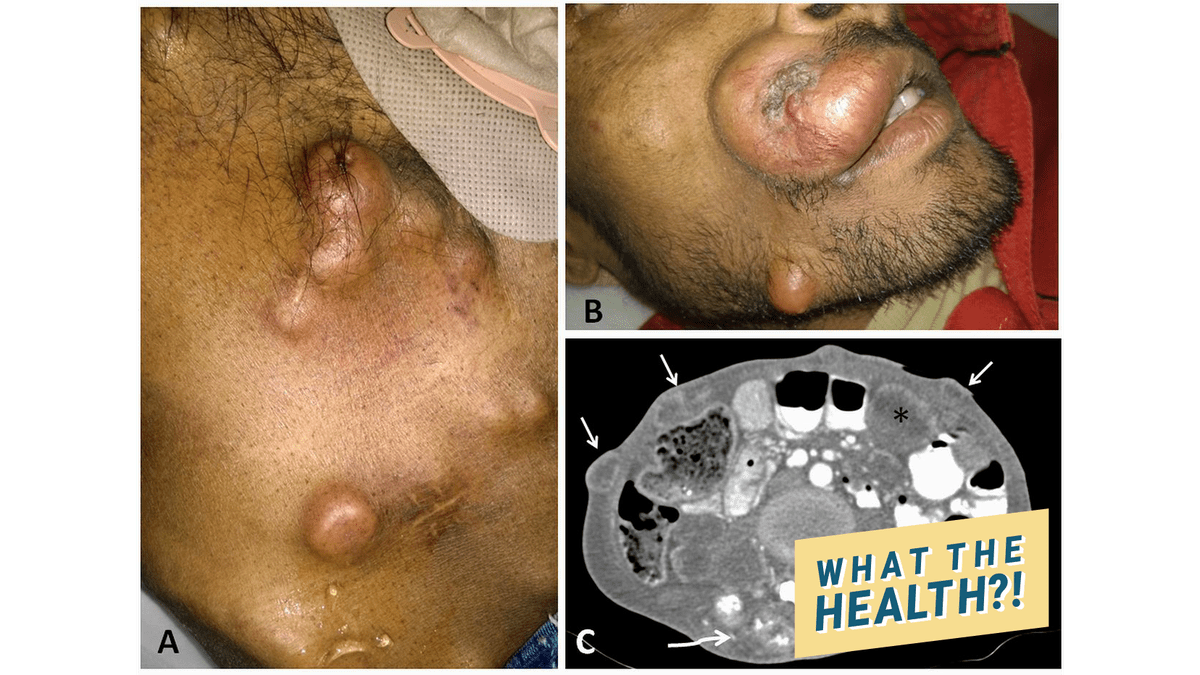 wth Cutaneous metastasis in adenocarcinoma rectum
wth Cutaneous metastasis in adenocarcinoma rectum
The spread of cancers to the skin is rare, according to the report. When it does happen, it's usually in lung cancer patients. However, this happens to 6% of colorectal cancer patients, the case report authors note. The abdominal wall is the most common site of cutaneous metastasis in colorectal cancer patients.
The spread of cancer to the skin usually occurs by way of veins or the lymphatic system, the report notes. It "is often detected several years after the surgical removal of the primary tumor, the mean interval being 33 months," the authors write.
They warn that doctors should evaluate any lumps on the skin that patients who have been treated for rectal cancer notice.
"Any cutaneous nodule in a postoperative case of adenocarcinoma rectum should be thoroughly evaluated as it may be the earliest sign of recurrence," the report says. "Cutaneous metastasis is usually a sign of distant dissemination, and such patients carry a poor prognosis."
RELATED: The Rectal and Colon Cancer Symptoms You Need to Know, Even if You're Young
]]>“Basically everyone has some risk,” Jennifer Christie, MD, clinical director of gastroenterology at Emory Clinic in Atlanta, tells Health.
Colorectal cancer (or colon cancer, for short) starts in the lining of the colon (aka the large intestine) or the rectum. In women, the lifetime risk of developing this cancer is just over 4%; in men, it’s 4.5%, according to the American Cancer Society (ACS).
While it’s not always clear what causes colon cancer, there are certain risk factors that can boost your odds of developing this disease.
Risk factors help determine when someone should start screening and how often, so talk to your doctor about your particular colorectal cancer risks.
RELATED: The Rectal and Colon Cancer Symptoms You Need to Know, Even if You’re Young
Your age
Colorectal cancer is most frequently diagnosed in people 50 and older. But youth does not give you a pass.
“We’ve seen patients here as young as 17 with colon cancer, so it’s not always the cancer of older people,” observes Benjamin Weinberg, MD, assistant professor of medicine in the Division of Hematology and Oncology at Georgetown University’s Lombardi Comprehensive Cancer Center in Washington, D.C.
Most young adult colon cancers occur in people in their 40s, according to the Colorectal Cancer Alliance. Nobody really knows why younger folks are developing colon and rectal cancer, adds Dr. Weinberg, who is conducting research to explore whether a person’s gut microbiome might play a role.
In 2018, the ACS called for screening to begin at age 45, instead of 50, in people of average risk, based in part on rising rates of colon cancer in young adults.
Your race or ethnicity
African Americans are not only at higher risk of developing colon cancer; they’re more likely to die from it.
“We don’t know why that may be, but we do believe that there may be genetic factors,” notes Dr. Christie. “And there also may be some dietary factors that may be playing a role,” she says.
The American College of Gastroenterology recommends screening African American men and women beginning at age 45.
People of Ashkenazi Jewish descent have one of the highest risks of colon cancer of any ethnic group in the world.
RELATED: The 12 Best Ways to Prevent Colorectal Cancer
Family history
Anyone with an immediate family member (a parent, sibling, or child) or several second-degree relatives (grandparents, aunts, and uncles) with colon cancer is at higher risk of developing the disease.
If colorectal cancer runs in your family, your doctor will likely recommend that you begin screening at an earlier age than someone at average risk.
It’s not clear whether an inherited risk, such as family history, makes someone more susceptible than a lifestyle risk, like your diet, but each poses an independent risk, Dr. Weinberg explains.
Personal history
If you’ve had pre-cancerous growths (called polyps) removed from your colon or rectum, you’re more likely to develop colorectal cancer.
Certain non-colon cancers, such as uterine or ovarian cancer, may also raise your risk for colorectal cancer.
“You should make sure you get appropriate follow-up [care],” says Dr. Christie, a member of the governing board of the American Society for Gastrointestinal Endoscopy.
RELATED: 16 Unexpected Cancer Symptoms Every Woman Should Know
A diagnosis of inflammatory bowel disease
People with the inflammatory bowel diseases Crohn’s disease or ulcerative colitis are at greater risk of developing colorectal cancer.
“Any time you have chronic inflammation, you have increased cell turnover. And every time a cell turns over, there’s a theoretical risk that it can develop a mutation,” explains Dr. Weinberg, a gastrointestinal oncology specialist.
Over time, he adds, some of these cellular defects can cause cancer.
An inherited syndrome
A number of different gene-based syndromes can boost your risk of developing colon cancer. Lynch syndrome is the most common hereditary cause of colon cancer. Another is familial adenomatous polyposis or FAP.
Of course, you might not know the genetics of your family’s colon cancer. “But if you have a cluster of colon cancers in your first-degree relatives or even a grandparent and then a cousin or aunt, then that sort of tells you something,” Dr. Christie says. “And that’s probably going to put you in the higher-risk category.”
RELATED: What Is Lynch Syndrome—and How Does It Increase Colon Cancer Risk?
A sedentary lifestyle
While there’s no proof that exercise actually lowers a person’s risk of colon cancer, studies show that folks who are inactive are much more likely to develop the disease than regular exercisers.
In fact, people who’ve previously had colon cancer removed are encouraged to exercise to reduce their risk of recurrence, Dr. Weinberg notes. “It doesn’t need to be running marathons,” he says. “It can even be just getting your heart rate up a few times a week.”
Certain dietary factors
What you eat can make a difference when it comes to your risk of colorectal cancer. A diet high in red meat and processed meat has been linked to higher rates of the disease.
Patients always ask Dr. Christie, “Doc, how can I reduce my risk? What should I eat?” In general, she says she recommends a high-fiber, low-fat diet, including plenty of green, leafy veggies.
RELATED: This At-Home Stool Test Is Just as Effective as a Colonoscopy
Being overweight or obese
It’s not just a high BMI that makes a difference. Carrying around excess belly fat is also linked to a higher risk of several different cancers, including colorectal cancer.
Drinking too much
Excess alcohol consumption is consistently linked to a higher risk of multiple cancers, including colorectal cancer, according to the American Society of Clinical Oncology.
To reduce this risk, women should limit their drinking to no more than one alcoholic beverage a day and men should stick to one to two drinks daily.
RELATED: I Went to the Doctor With Stomach Pains—and Found Out I Had Stage 4 Colon Cancer
Smoking
Tobacco use isn’t just toxic to the lungs. If you’re a longtime smoker, you’re more likely to die from colon cancer than a non-smoker, according to the ACS.
A large Norwegian study found women and men who had ever smoked had a 20% increased risk of death from colorectal cancer compared with people who had never smoked.
Having type 2 diabetes
Even after accounting for being overweight and sedentary, people with type 2 diabetes have a higher risk of developing colon cancer, according to the ACS.
Oftentimes, people who have diabetes have higher levels of insulin circulating in their blood, which may stimulate cancer growth, Dr. Christie notes.
]]>The American Cancer Society (ACS) did just that—in 2017, after reporting a dramatic uptick in colorectal cancer cases in younger adults, the ACS suggested testing for the cancers should begin at age 45 rather than 50 for people at average risk of the disease.
 Colon-Cancer-Screening-Options-GettyImages-1125831054 (CDC) and the US Preventive Services Taskforce, however, maintain that colorectal screenings may continue to begin at age 50, as long as the person is of average risk for the disease. People may stop those regular screenings at the age of 75, and then after the age of 85 no one needs colorectal cancer screenings, per the ACS.
Colon-Cancer-Screening-Options-GettyImages-1125831054 (CDC) and the US Preventive Services Taskforce, however, maintain that colorectal screenings may continue to begin at age 50, as long as the person is of average risk for the disease. People may stop those regular screenings at the age of 75, and then after the age of 85 no one needs colorectal cancer screenings, per the ACS.
RELATED: 7 Colorectal Cancer Treatments and Therapies, Explained by Doctors
Those who should begin colorectal cancer screenings before the age of 50 or 45 are people with an increased risk of being diagnosed with the disease, like those who have the following: a family history of colorectal cancer, a personal history of colorectal cancer or polyps, a personal history of inflammatory bowel disease (IBD, either Crohn's disease or ulcerative colitis), certain genetic conditions (familial adenomatous polyposis or hereditary non-polyposis colorectal cancer), or a history of radiation to the abdomen or pelvis, per the ACS.
But even if you haven't hit the typical age when screenings start, or don't have any factors that could increase your risk of the disease, it's imperative to stay aware of your body and to bring any alarming colorectal cancer symptoms to your doctor immediately. Those include signs like blood in your stool, unexplained stomach cramps, weight loss, or changes in your bowel habits.
Regardless of why you're getting screened for colorectal cancer, it's important to know what you're getting yourself into. Here's what you need to know about your colorectal cancer screening options—and who should get what kind.
Types of colorectal cancer screening tests
If a colorectal cancer screening test conjures up images of colonoscopies and bowel prep strategies, you may be able to breathe a sigh of relief: The US Preventive Services Task Force actually outlines six different screening options—and three of them don't include any type of out patient procedure at all.
Stool tests
The CDC lists three different stool tests that can be used for colorectal cancer screenings—something that could lead to more people getting screened for colorectal cancer overall. "If we give patients a choice and let them factor in what's available to them, then maybe those things will contribute to higher adherence and therefore greater practical impact of the screening recommendation," Nancy You, MD, an associate professor in the Department of Surgical Oncology at the University of Texas MD Anderson Cancer Center, tells Health.
Those stool-based tests include: the guaiac-based fecal occult blood test (gFOBT), which uses a chemical called guaiac that can detect blood in your stool; the fecal immunochemical test (FIT), which also can detect blood in your stool, this time through the use of antibodies; and the FIT-DNA test, which is part-FIT, part DNA test that can detect altered DNA in your stool.
Both the gFOBT and FIT tests only require you to collect small sample of stool, which is then sent to a lab. They're meant to be done once a year. The FIT-DNA test, on the other hand, requires you to collect an entire bowel movement, but only needs to be done every three years.
Here's the thing about stool-based tests though: They may be easier to do, but if you get a positive (or even inconclusive) result, you will still have to get a colonoscopy done, according to the ACS. And these less invasive tests aren't recommended for those with a higher risk of developing colorectal cancer.
RELATED: What Is a Colonoscopy? From Prep to Recovery, Everything you Need to Know About the Procedure
Flexible sigmoidoscopy
Think of a flexible sigmoidoscopy as a less intense version of a full-blown colonoscopy. A doctor will use a short, thin, flexible tube into your rectum to check for polyps or cancer— but only inside the rectum and lower third of your colon.
A flexible sigmoidoscopy is often preferable to a colonoscopy because they may take less time and may not require anesthesia, per the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). It may also let you avoid a complete bowel prep, per the ACS, but that's entirely up to your doctor performing the procedure. It's recommended that a flexible sigmoidoscopy is done every five years, or every 10 years in addition to an FIT stool test each year.
As with stool tests, if your doctor detects abnormalities in your flexible sigmoidoscopy, you will likely need another full colonoscopy to check the rest of your colon. A flexible sigmoidoscopy is less recommended for those with a heightened risk of colorectal cancer.
CT colonoscopy
A computed tomography (CT) colonoscopy is a type of virtual colonoscopy—that means it uses X-rays and computers to show doctors your entire colon, without physically inserting a scope into your body.
This option is still pretty new, which means that it may not be available via your gastroenterologist, and if it is, insurance may not cover it. This may seem like the easier route—you don't need sedation, and it shows your entire colon on a screen—but you will still have to do a full bowel prep for the procedure. If your doctor sees a polyp or anything else abnormal, you'll also need to have an additional colonoscopy done to further test for cancer. A CT colonoscopy can be performed every five years, as long as you continue having clear results.
RELATED: 12 Colorectal Cancer Risk Factors to Know About
Colonoscopy
A colonoscopy is the gold standard for colorectal cancer screenings. During the procedure, doctors will insert a long, thin, flexible tube into your rectum and throughout your entire colon to check for polyps or cancer. If a doctor does find something abnormal during a colonoscopy, they can quickly remove the polyp or tissue sample to test for cancer. You will likely be under anesthesia for the procedure, and may also miss a day of work for recovery.
A colonoscopy brings an added element of discomfort: bowel preparation. According to the American Society for Gastrointestinal Endoscopy, there are different types of bowel preps (your doctor will prescribe the one best for you and your situation), but it will generally include a diet limited to clear fluids for at least one day before your colonoscopy. Along with a change in diet, you will also receive a prescription for medication that will more thoroughly cleanse your colon of waste.
Is it uncomfortable? Sure, but it's the best way for your doctor to thoroughly examine your colon and not miss any precancerous growths or other abnormalities. If your colon isn't as clean as your doctor would like, they may make you do it all over again, so you may as well do it right the first time to sidestep that.
A colonoscopy is recommended for those who have a higher risk of colorectal cancer, regardless of their age. For those who are at an average risk of the disease, colonoscopies can be performed every 10 years.
Talk to your doctor to help you determine which colorectal cancer screening method is right for you and to get the details on how often to screen, which, again, varies by test. You'll also need to check which tests your insurance will cover.
And in addition to screening for colorectal cancer, it's also important to do all you can to take healthy steps that might lower your lifetime colorectal cancer risk, such as cutting back on red meat and alcohol, eating plenty of high-fiber produce, getting regular exercise, maintaining a healthy weight, and quitting smoking if you haven't already.
To get our top stories delivered to your inbox, sign up for the Healthy Living newsletter
]]>“It’s extremely rare for an incidence of a disease to increase this much,” says Andrea Cercek, MD, a gastrointestinal oncologist at Memorial Sloan Kettering Cancer Center.
A 2019 study further confirms that the incidence of colorectal cancer is getting more prevalent: The number of people diagnosed with colon cancer under the age of 50 has risen from 10% in 2004 to 12.2% in 2015. According to the research, which was published in the American Cancer Society journal Cancer, when younger patients are diagnosed, the disease is more likely to have advanced to stages three or four.
RELATED: 16 Unexpected Cancer Symptoms Every Woman Should Know
Researchers aren't yet sure what's behind the rise, but they have some theories. For one, the same lifestyle factors contributing to the growing obesity epidemic are also associated with colorectal cancer. “It’s likely that some of the behaviors that contribute to obesity, like a sedentary lifestyle and poor diet, like high consumption of red and processed meat, and a low consumption of milk products, lead to [colorectal cancer]," says Rebecca Siegel, MPH, lead epidemiologist on the 2017 study. Some researchers are also exploring the connection between gut microbiome changes and cancer, but have yet to determine any direct link, says Dr. Cercek.
Based in part on these findings, the American Cancer Society lowered the screening age for colorectal cancer to 45 for people with average risk (meaning they have no family history of the disease). Other groups continue to advise starting colonoscopies at age 50.
Meanwhile, both Siegel and Dr. Cercek say it's smart to keep an eye out for colorectal cancer symptoms. Many of the signs of colorectal cancer are easy to ignore or shrug off as something minor—and young people are especially prone to dismissing them, says Dr. Cercek. “They think it’s not a big deal and they’re too busy working and living their lives, and they’re more likely to be diagnosed at a later stage.”
Here are the colon cancer symptoms Dr. Cercek and Siegel say you shouldn't ignore:
- Blood in the stool (which can be bright red or dark)
- Bleeding from the rectum
- Abdominal cramping (that can’t be explained by a bug or something you ate)
- A change in your bowel movements—whether that’s in timing, frequency, shape of stool, or amount of stool
- Persistent constipation or diarrhea
- Unexplained weight loss
If you experience any of these symptoms of colon cancer for more than a week, it’s time to talk to a doctor. Do your homework before your appointment and find out if you have a family history of colorectal cancer—if you do, it may prompt your doc to screen you, says Dr. Cercek.
RELATED: 8 Things You Need to Know About Your Colon
Siegel warns, however, that if you feel brushed off by your MD, you may need to push for further screening. “Most young people will just have some blood in their stool, and it will be diagnosed as hemorrhoids, which is the most likely thing,” she says. “But we need to raise awareness among physicians that these symptoms need to be followed up.”
Dr. Cercek agrees. “Say, ‘There’s data that colorectal cancer rates are rising in young people, and these symptoms are concerning to me. Should I get a colonoscopy?’” she suggests. Colonoscopies are used to search for polyps or other masses that can become cancerous.
You can lower your risk of colorectal cancer by eating a healthy diet with lots of fruits, vegetables, and fiber, and cutting down on red and processed meats. Milk has also been shown to help lower risk, says Siegel. Exercise and maintaining a healthy weight will also help protect you from rectal and colon cancer.
“Know your body and know the colorectal cancer symptoms, and live a healthy and active lifestyle,” says Siegel. “Those are the things we can do right now to help avert risk.”
This post was originally published on March 3, 2017 and updated for accuracy.
]]>Most health organizations recommend that a colonoscopy be performed at least once every 10 years starting at age 45 or 50. But studies in recent years have suggested that a less expensive, less invasive, at-home stool screening may be as effective as colonoscopy at detecting cancer. And now, researchers say, a review published this week in the Annals of Internal Medicine provides the strongest evidence yet that many patients can safely forego colonoscopy in favor of this once-a-year, easy-to-use test.
RELATED: Colorectal Cancer Screenings Should Start at 45, New American Cancer Society Guidelines Say
Known as fecal immunochemical tests (FIT), these at-home kits analyze stool samples and identify hidden blood that could be a sign of cancer. For the new review, researchers from Indiana University School of Medicine and the Regenstrief Institute in Indianapolis combed through the findings of 31 previous studies involving 120,255 participants, all of whom were given an FIT and then a subsequent colonoscopy.
When the results were combined and analyzed as a whole, the researchers found that about a third of patients who received positive results on their FIT were found to have colorectal cancer or an advanced precancerous polyp. What this means, the researchers say, is that FIT can be a good “pre-screening” test for adults who are at average risk and have no symptoms, and can save people the hassle and costs of more complicated testing.
“If annual FIT results remain negative, FIT buys you time until colonoscopy may be required,” said lead author Thomas Imperiale, MD, professor of gastroenterology at Indiana University School of Medicine, in a press release. “And it could be the case that a colonoscopy for screening may never be necessary or required.”
RELATED: The Rectal and Colon Cancer Symptoms You Need to Know, Even if You're Young
According to an editorial published with the review, colonoscopy is considered the gold standard for colon cancer screening in the United States; it’s also the most frequently used screening method, and is often given to healthy adults with no symptoms or risk factors. But in several other countries, the test is only performed if a patient’s FIT results are positive.
“It should be reassuring to skeptics that most countries with [colorectal cancer] population screening programs use FITs as their test of choice,” wrote editorial author James Allison, MD, a professor emeritus at the University of California, San Francisco. “For example, in Canada, a positive FIT result is mandatory in an average-risk patient before colonoscopy is covered by insurance.”
FIT is also considered an effective pre-screening in the United Kingdom and Italy, as well, according to the review. A similar approach could be safely adopted in the United States, says Dr. Imperiale. But a better system to actually get people tested (and ensure they get a follow-up colonoscopy, if their FIT is positive) is still needed, he points out. “We need a system that is population-based rather than the current opportunistic one,” he said in the press release, noting that poor, uneducated, and uninsured patients are often left out.
In 2018, the American Cancer Society updated its colorectal cancer guidelines, recommending that screening start at age 45 (instead of 50) and continue through age 75 or 85, depending on patient preference and prior screening history. The options for screening, according to these guidelines, include colonoscopy every 10 years, a fecal blood test (such as FIT) every year, or various other procedures (a stool DNA test, colongraphy, or flexible sigmoidoscopy) every 3 to 5 years.
In his editorial, Dr. Allison stresses that it’s important for doctors to see FIT as equal to colonoscopies, and not as a second-rate test. “Physicians in the United States must understand the advantages of FITs as screening tests for [colorectal cancer] and educate and advocate to increase screening rates,” he wrote, “especially in vulnerable populations."
RELATED: What It Was Like to Be Diagnosed With Colorectal Cancer When I Was 28 Weeks Pregnant
]]>